For many people with HIV, the COVID-19 pandemic seems all too familiar: the fear, the stigma, the loss of loved ones, the disproportionate impact on marginalized communities and a federal government that has failed to adequately respond to the crisis.
“Again, there’s a sense of existential dread—a low-grade panic,” says blogger and activist Mark S. King.
This fear is compounded by uncertainty. People with HIV wonder whether they’re more likely to contract the coronavirus (officially known as SARS-CoV-2) or are at greater risk of becoming seriously ill. Will the crisis affect their ability to access HIV care and services? And how will they deal with the disruption of normal life, the social isolation and the financial fallout of the pandemic?
Istock
HIV and COVID-19 Risk
Typically, people with compromised immune systems are more susceptible to a variety of infections. Early reports from China, where the COVID-19 outbreak first emerged late last year, indicated that people with immune suppression were more likely to become seriously ill if they acquired the coronavirus.
What’s more, nearly half of people living with HIV are over 50—the risk of severe COVID-19 rises with age—and many have underlying health conditions associated with worse outcomes, such as diabetes, high blood pressure, chronic lung disease or cardiovascular disease.
But so far, experts agree that people on antiretroviral treatment who have an undetectable HIV viral load and a near-normal CD4 count do not appear to be at higher risk than their HIV-negative counterparts.
“My sense from the accumulating evidence is that incidence rates might be lower than expected,” says Steven Deeks, MD, a professor of medicine at the University of California at San Francisco. “I personally think that’s because people with HIV were well aware of how to protect themselves and educated about the nature of the epidemic, and they responded pretty quickly.”

Steven Deeks, MDCourtesy of Jan Brittenson
In one of the first reports about COVID-19 in people with HIV, researchers contacted 1,178 HIV-positive people in Wuhan, China. Eight people with symptoms were found to have COVID-19. Six of them had mild cases, one had severe disease and one died. Among the remaining asymptomatic people, just one of the nine individuals known to have had close contact with COVID-19 patients tested positive for SARS-CoV-2.
In another early report, Spanish researchers found that among the first 543 people admitted to a Barcelona hospital with the new coronavirus, five were HIV positive. Three had mild or moderate disease, and they recovered and were released from the hospital within about a week. One person, who was not on HIV treatment and had a CD4 count of 13, received supplemental oxygen and recovered. The oldest man (age 49) was put on a ventilator and remained hospitalized.
A related study from Italy identified 47 people known or suspected to have the coronavirus out of nearly 6,000 people with HIV followed at a hospital in Milan. They were less likely to have advanced respiratory disease or to be hospitalized than HIV-negative people, and only two died. But the researchers noted that the HIV-positive group was about 10 years younger, on average, than HIV-negative patients with severe COVID-19.
In contrast, a report from Germany described 33 HIV-positive people diagnosed with COVID-19; all of them were on antiretrovirals with an undetectable or low HIV viral load. Fourteen were hospitalized, six required intensive care and three died—higher rates than those observed for German COVID-19 patients overall—but ultimately, 91% recovered.
Turning to the United States, researchers identified 43 HIV-positive people (0.8%) among 5,700 patients hospitalized with COVID-19 in New York City—where about 1% of the population is living with HIV—indicating that HIV itself does not appear to be a risk factor. A separate analysis compared 21 HIV-positive and 42 HIV-negative people with COVID-19. Although the HIV group had somewhat higher rates of intensive care admission, use of ventilators and death, these differences were not statistically significant, meaning they could have been due to chance.
“We thought maybe we were going to see it more in people living with HIV because there are these clear risk factors, but we haven’t seen people with HIV coming into the hospital more or having more severe COVID-19 at all,” says Monica Gandhi, MD, MPH, the medical director of Ward 86, the HIV clinic at Zuckerberg San Francisco General Hospital, where most patients have well-controlled virus.

Monica Gandhi, MDCourtesy of UCSF
Taken together, these early studies and anecdotal reports suggest that HIV-positive people—at least those on effective antiretroviral therapy—are not a high-risk group based on their HIV status alone. As a result, interim guidance from the Department of Health and Human Services states, “People living with HIV who are diagnosed with COVID-19 have an excellent prognosis, and they should be clinically managed the same as persons in the general population with COVID-19, including when making medical care triage determinations.”
The World Heath Organization (WHO) concurs: “At present, there is no evidence that the risk of infection or complications of COVID-19 is different among people living with HIV who are clinically and immunologically stable on antiretroviral treatment when compared with the general population.”
However, the jury is still out on people with HIV who are not taking antiretrovirals and those who are on treatment but have not experienced good CD4 recovery. Around 40% of diagnosed HIV-positive people in the United States do not have viral suppression, and the 15% of individuals who remain undiagnosed are, of course, not on treatment.
Are People with HIV Protected?
Findings like these actually raise the opposite question: Are people living with well-controlled HIV—and potentially those taking antiretrovirals for pre-exposure prophylaxis (PrEP)—somehow protected against COVID-19?
Preliminary data suggested that some HIV medications might help control the new coronavirus, as certain antiretrovirals have shown activity against SARS-CoV-2 in the laboratory. Tenofovir disoproxil fumarate (one of the drugs in Truvada, used for HIV treatment and PrEP) appears to have both antiviral and immune-modulating effects. And during the 2003 SARS outbreak, caused by a related coronavirus, some patients improved after being treated with the protease inhibitor combination Kaletra (lopinavir/ritonavir).
But so far, studies in humans have not yielded much evidence that this is the case. In fact, most HIV-positive people who have developed severe COVID-19 were on antiretroviral treatment.
One of the first randomized clinical trials of Kaletra for COVID-19 found that it is no more effective than standard supportive care, although it may offer some benefit for those treated early. And the company that manufactures darunavir (Prezista and Prezcobix) cautioned that it is unlikely to have much activity against SARS-CoV-2.
Nonetheless, at least a dozen clinical trials of antiretrovirals for COVID-19 are underway, including WHO’s large Solidarity trial and a Spanish study evaluating whether Truvada might help prevent SARS-CoV-2 infection or lessen disease severity in health care workers.
Until more is known, experts advise against switching antiretrovirals in an effort to prevent or treat COVID-19, and they stress that people living with HIV and those using PrEP should take all the same precautions recommended for the general population to guard against the coronavirus.
COVID-19 and Your Immune System
Another avenue of exploration relates to the fact that COVID-19’s serious lung and other organ damage is largely caused by the immune system’s response rather than by the coronavirus itself. In the most severe cases, an immune overreaction known as a cytokine storm floods the body with chemical messenger proteins that trigger excessive inflammation. If the immune system is causing the damage, some wonder, could modest immune suppression actually be an advantage?
“Some people have speculated that maybe it even helps to not have your immune system work perfectly,” Gandhi says. “Maybe if you’re a little immunosuppressed, your inflammatory response may not be as crazy and out of control.”
But it’s too simple to talk about strong or weak immunity overall. The immune system is made up of multiple parts, and they do not always work in sync.
Natural killer cells, macrophages and other first responders provide the initial line of defense against invaders. CD4 or helper T cells—the familiar targets of HIV—orchestrate immune responses, while CD8 or killer T cells attack virus-infected cells, and B cells produce antibodies. Cytokines released by immune cells serve as the means of communication to coordinate the whole process.
“Everything I know about how HIV affects the immune system suggests that people with HIV would be more likely to have poor control of the coronavirus early on and have more inflammation-associated problems later,” Deeks explains. “There is immune suppression on one end when you want a better response and perhaps too much poorly regulated inflammation on the other end when you want things to calm down.”
Both T cells and B cells play a role in fighting SARS-CoV-2, but antibody production is currently what’s on everyone’s mind. If antibodies can prevent reinfection, that could allow people who have become immune to safely resume social and economic life.
“So far, it looks like anyone who has been exposed probably is going to get antibodies,” says Gandhi, “but it’s possible that in immunosuppressed patients—and even people living with well-controlled HIV—this may take longer.”
Scientists have already made remarkable progress in understanding COVID-19, but much remains to be learned. “We don’t know what kind of antibody response is protective. We don’t know what kind of responses we want to generate with vaccines. We don’t know how long they’ll last. And we don’t know whether or not people with HIV or cancer are going to have a less robust antibody response,” says Deeks. “These are the billion-dollar questions that the world is trying to answer.”
When it comes to treatment, he adds, “The ideal thing would be a benign, orally available drug that has a potent effect on the virus, is safe and is not susceptible to viral resistance and that can be made for pennies and would be easy to distribute widely. We don’t have anything on the shelf like that, so we need to start at the beginning.”
The antiviral drug furthest along in the pipeline, Gilead Sciences’ remdesivir, must be given by IV infusion, though injectable and inhaled formulations are being studied. Hydroxychloroquine, an old drug touted by President Trump, appears to have modest activity at best, and it can cause fatal heart problems. Medications that dampen the immune response can help some people with advanced disease, but it would be better to prevent cytokine storms in the first place.
COVID-19 PrEP also holds potential. “In a prevention setting, you might see a fair amount of benefit with drugs that only have modest activity,” Deeks says. “It may be that for prevention, you don’t really need something super powerful just to block transmission.” Although they would be more difficult and expensive to produce and administer than pills, Deeks thinks long-acting antibodies against SARS-CoV-2 might be “the kind of thing that you’d want to give a health care worker in the middle of a hot zone.”
Don’t Neglect HIV
COVID-19 is currently the hot topic for virologists, immunologists and epidemiologists worldwide. In fact, many of the top names in the HIV field—all the way up to National Institute of Allergy and Infectious Diseases director Anthony Fauci, MD—are applying the lessons they’ve learned from HIV to the latest pandemic.
“The massive investments that the National Institutes of Health has made into HIV research are paying off in amazing ways in terms of our capacity to deal with this new epidemic,” Deeks notes.
But many researchers, public health officials and advocates are concerned about the diversion of resources from the domestic and global HIV/AIDS response to COVID-19.
WHO and the Joint United Nations Programme on HIV and AIDS (UNAIDS) have warned that disruptions in HIV services and access to antiretrovirals could lead to more than half a million extra AIDS-related deaths, an increase in new HIV infections and a steep rise in mother-to-child HIV transmission in sub-Saharan Africa by the end of next year.
“The COVID-19 pandemic must not be an excuse to divert investment from HIV,” says UNAIDS executive director Winnie Byanyima. “There is a risk that the hard-earned gains of the AIDS response will be sacrificed to the fight against COVID-19, but the right to health means that no one disease should be fought at the expense of the other.”
In the United States, in an effort to both protect patients and reduce the demand on health care systems, experts initially urged people with HIV to utilize telemedicine and minimize in-person medical visits—for example, by delaying viral load monitoring. But this is not a viable long-term approach as the COVID-19 pandemic stretches into its sixth month.
“People with HIV went into hiding, but we need to get them back into the clinics. We need to start doing viral load measurement and make sure they have access to treatment. We need a balance between staying out of the health care system and engaging with the health care system,” says Deeks. “I think we’ll be doing a lot more telemedicine in the future, and for a lot of my interactions with my patients, it’s been fine. But I know people who I should be seeing in person much more frequently.”
Numerous efforts are underway to learn more about COVID-19 in people with HIV. For example, Jeff Taylor, a longtime treatment activist and advocate for long-term survivors, is working on a study that aims to follow a cohort of HIV-positive and well-matched HIV-negative people age 50 or older to see who gets the coronavirus, what kind of immune responses they mount and what the course of disease looks like over time.
“An important part of that will be studying the psychosocial impact of COVID-19 to see if this triggers posttraumatic stress disorder from the AIDS pandemic, how well people cope and if there are unique kinds of stigma associated with COVID-19 among people who are more vulnerable and may need to continue to remain socially isolated even after things reopen,” Taylor says.
Gandhi is also worried about the financial impact of the shutdown and the effects of social isolation—especially on older people and those struggling with mental health or substance use issues—as well as the reemergence of the same disparities long familiar to people living with HIV.
“COVID-19 has basically proven again that we haven’t fixed our structural inequities, structural racism, homelessness and all of the other unfair things that happen in society,” she says. “We’ve been shouting this from the rooftops since the beginning of HIV. It’s important for all of us as advocates to change the equation.”
CATCHING A BREAK
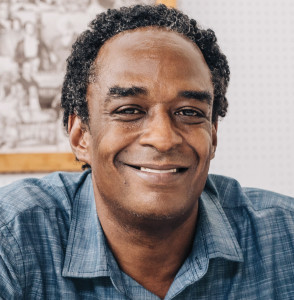
Art Jackson’s experience living with HIV has
helped him face the challenges of COVID-19.
On the first weekend in March, Art Jackson, 55, lost his sense of taste. He soon started to have intense headaches and chest congestion. But his experience living with HIV for three decades stood him in good stead.
“One of the things about being HIV positive is that we know our bodies. We know when something is wrong,” Jackson says. “I’ve been very proactive about my health. When I started getting congested in my chest, I said, ‘This is not cool.’”
Art JacksonJillian Clark
After a friend he had spent time with about a week and a half earlier got sick and tested positive for the new coronavirus, he got tested too, with the same result.
“My congestion started getting really bad when the sun was about to go down, and by the time it was dark, it felt like someone was standing on my chest,” he recalls. “My body was hurting from the toes on up.”
Jackson, who has long had undetectable HIV and a high CD4 count, participated in telemedicine visits with his doctor via Zoom, but he didn’t want to go to the hospital because “friends who were going in were dying.” Instead, his doctor or a nurse would call to check on his breathing every few hours. He managed his symptoms with over-the-counter medications and breathing in steam from a pot of hot water with lemons.
“A couple nights, I really thought I wasn’t going to make it. It took all my energy just to go into the kitchen,” he says. “The virus wanted me to lie down, so I said I’m going to get up and walk and try to give my lungs a chance. I thought about my grandmama and mama and aunties and their home remedies, and I did what I knew I had to do.”
Jackson, who lives alone, also knew to call on loved ones for support. “People in my life weren’t going to let me go under,” he says. “I have an amazing family and a network of people who love and care about me. I have some amazing friends who called me in the middle of the night and made me laugh. They knew I needed that connection and needed to hear they cared about me.”
After about seven days, his symptoms started to ease up. But things still are not back to normal. “I still feel a little off-kilter. I still get winded. Even now, I would say I’m at about 80%. It’s a gradual process,” he says.
In addition to his own battle with the coronavirus, Jackson has lost three family members and four friends to COVID-19.
“It’s brought back so much of the trauma of HIV in the ’80s and ’90s—the stigma, the fear, but especially the deaths,” he says. “It’s brought back survivor’s guilt and wondering why I’m still here. For others, this is new, but we’ve dealt with a plague before.”
What’s more, Jackson has faced hurtful attitudes from others about having had COVID-19. “Fear just breeds stigma,” he says. “Now we’ve got to educate people. For some reason, this is something I’ve been charged to do, and I’m OK with that.”
He’s also felt the financial impact of the pandemic. After waiting weeks for unemployment assistance with no relief in sight, Jackson, who recently moved from Indianapolis to Charlotte, North Carolina, landed a new job as an HIV prevention coordinator with the Carolinas CARE Partnership.
“I’m not a religion person, but I believe in faith and grace, and I’m grateful for my blessings,” he says. “Sometimes it seems unfair. I’ve lived with HIV longer than I lived without it, and I wonder, When can I catch a break? But my break was to make it through, because many people didn’t.”







3 Comments
3 Comments