T-20 (pentafuside)
Each Dose Contains:
36 amino acids
74-step process
7 years R & D
60 million $$$
In Stores: 2002
Right now it’s one day at a time in HIV treatment land: behind us, the dashed hopes of eradication; up ahead, gathering fears about protease side effects. Once burned and twice shy, HIVers have learned to be grateful for the health they do have and careful not to expect too much from the drug pipeline.
Enter T-20, the first in a new class of anti-HIV drugs to enter Phase III trials. (An earlier contestant, Peptide T, is still slouching toward funding and recognition.) What’s new? Rather than attacking HIV once it’s inside a cell, T-20 is quicker on the draw, zapping the virus before it even enters a cell. Even better, it’s reportedly less toxic than other anti-HIV drugs. In this dry spell, advocates are touting T-20 as the pipeline’s “next big thing.” Indeed, the drug is a valuable addition -- not just another copycat -- to the AIDS arsenal. For HIVers at the end of their hope, it may even be a lifesaver as salvage therapy.
But the current sober mood may be the best way to welcome T-20. After all, a new class of drugs does not a cure make. So, great expectations? Not quite. Yet perhaps this product will prove us wrong.
Good luck, hard work and big bucks took this fusion inhibitor from a gleam in a researcher’s eye to a compound coursing through the blood of HIVers. Its difficult development is a case study in why, even in this age of rational drug design, only one out of 1,000 compounds makes it to market.
Chapter 1
In which vaccine hunters bring home a foundling
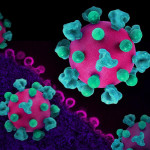
Our story starts in 1990 when scientists first broke the code on how HIV fuses with human cells. Wes Craven couldn’t have directed a spookier scene: In order to insert its genetic material into a CD4 cell, the virus must grab onto it by binding with the cell’s surface. The “spikes” on HIV’s envelope are two proteins known as gp120 and gp41. First, the gp120 binds to CD4, and then, faster than you can say Sigourney Weaver as Ripley, gp41 uncoils like a spring-loaded harpoon to pierce the cell’s membrane. Next, gp41’s two peptides draw together, pinning the virus and the CD4 cell together while HIV inserts its deadly genetic material.
It was this moment of fusion that fascinated Dani Bolognesi, PhD, and his HIV vaccine team at Duke University’s Center for AIDS Research. They screened compound after compound, searching for a chemical wrench that could cause the viral machinery to break down at this point. Thomas Matthews, PhD, a member of the Duke team, thought that HIV’s gp41, in particular, looked good as a potential vaccine target, and during his investigations, he took a closer look at a compound dubbed T-21, a synthetic match for one of gp41’s peptides. “It was a case of serendipity,” Bolognesi says. “Tom decided to throw it in a culture with HIV, and sure enough, it had very potent activity against viral fusion.” So even though T-21 turned out to be a vaccine bust, it got a thumbs-up as a possible anti-HIV treatment. Yet as they developed T-21, the Duke researchers found that matching the other gp41 peptide made for an even better fusion blocker. This 36-amino-acid peptide -- named T-20, or pentafuside -- fits like a jigsaw-puzzle piece into the part of gp41 of which it is a copy, rendering it nonfunctional.
T-20’s discovery, says Bolognesi, “excited some investors” eager to back a brand-new class of anti-HIV drugs, and in 1993 he cofounded a new company called Trimeris and won an exclusive license from Duke University to develop the newly patented fusion-inhibitor technology. The firm, in North Carolina’s high-tech nexus, Research Triangle Park, went public in October 1997, raising some $34 million in seed money. Today, Bolognesi is president and CEO, Matthews is senior VP of research and development, and the once-tiny lab boasts 75 employees.
Chapter 2
In which naysayers advise Trimeris to abandon its baby
Three potential qualities made T-20 a dark horse the Trimeris team wanted to bet on. First, because of how it works -- it keeps HIV from getting inside a cell, unlike the nucleoside analogs and protease inhibitors, which kick in only post-penetration (see “The Shooting Gallery”) -- T-20 seemed likely to cause fewer complications than the current arsenal. Second, gp41’s “highly conserved” nature -- it appears virtually unchanged across various strains of HIV -- makes it relatively essential to viral function, suggesting to researchers that any mutations T-20 might cause would be weak. If so, then T-20, unlike most current anti-HIV meds, could be slow to trigger viral resistance. Third, it might, if nothing more, be effective as part of salvage therapy for HAART-resistant folks.
Yet the same novel aspects that excited Trimeris raised doubts in others, and the push for T-20 was straight uphill. According to Bolognesi, the prospect of developing a peptide “scares people. A lot of things can go wrong with a peptide in the body. In the beginning, many didn’t think we could do it.” Sam Hopkins, PhD, Trimeris’ director of clinical development, says the group pushing the drug worried that T-20 would last only seconds or minutes in the boodstream, and were “stunned” when it could still be detected hours after injection. With this advance, Hopkins says, “a small group of us looked at each other and said, ’This is going to work.’” “T-20 has behaved itself remarkably well,” Bolognesi says. “Nature has been kind.”
Not all the R & D troubles could be traced back to the mystery under the microscope. Early on, Bolognesi and Co. were confronted by two very practical questions: Could Trimeris find the money and the means to make enough of the compound to get it into clinical trials? And would HIVers be willing to take the drug as required -- through twice-daily, big-dose, painful, under-the-skin injections. (The peptide can’t be taken in pill or capsule form because acids in the stomach destroy it.) “We had to challenge pharmaceutical-industry dogma that all drugs must be orally available,” says Hopkins. The true test, of course, will take place once T-20 is widely available, but more than 100 HIVers are currently shooting up in clinical trials. Project Inform’s Martin Delaney believes that the needle barrier may be less formidable than expected. “People in advanced disease are often quite willing to tolerate a few daily injections, yet are very intolerant of swallowing noxious handfuls of pills,” he says. “For many, it is a more than reasonable trade-off.” However, not everyone is so confident, including apparently Trimeris itself, which has sought to downplay the injection issue.
Chapter 3
In which T-20 is not the prettiest pill at the party, but attracts attention anyway
Trimeris’ early test-tube studies showed that T-20 is a potent fusion fighter. Trimeris and the Food and Drug Administration (FDA) presented this early data at the International Conference on AIDS in Vancouver in June 1996, providing what, in a slow year, would have been a top-story glimpse of a groundbreaking weapon. But in the media blitz that met the conference’s debut of protease inhibitors, T-20 was reduced to a footnote.
Next up for Trimeris was to test the drug in animals. The FDA requires a mountain of data on safety, efficacy and pharmacology before green-lighting a drug for use in humans. Rarely does a compound’s success in the cell cultures and viral proteins of a test tube translate into success in a living being. Absorption can be a problem, as can metabolism. Short-term side effects are likely to materialize. Yet once again, T-20 exceeded expectations -- it protected the human immune cells in genetically engineered mice from HIV infection.
Boasting the FDA’s “Investigational New Drug” (IND) stamp of approval, T-20 went on to be tested in Phase I volunteers by some of the biggest names in AIDS research. In September 1997, retrovirologist Michael Saag, MD, from the University of Alabama at Birmingham reported positive data about T-20’s safety, efficacy and dosing in a trial of T-20 in 16 off-therapy HIVers. “The antiviral activity of fusion inhibitors appears to be as promising as protease inhibitors were at a similar stage of their development,” Saag said. In the cautious diction of science, this was the equivalent of a gushing endorsement.
Chapter 4
In which Trimeris must own up to some parental disappointments
Soon, Joseph Eron, MD, of the University of North Carolina at Chapel Hill got the first Phase II investigations up and running. In February 1999, he presented data clarifying T-20’s potential as salvage therapy. In this trial, 78 hard-case scenarios -- HIVers with high viral loads and multiple drug failures -- got T-20 for 16 weeks. The results? Nine out of 10 saw their HIV fall ... but soon creep up again. This red flag cautioned researchers that T-20 might have to be combined with other anti-HIV meds to sustain a long-term antiretroviral effect.
Last September, Jay Lalezari, MD, of Quest Clinical Research in San Francisco, put T-20’s salvage capacities to the test: 55 HIVers, over 90 percent of whom had virus resistant to protease inhibitors, nukes and non-nukes. Volunteers received twice-daily injections of T-20 as part of a HAART combo. After 16 weeks, 60 percent saw a significant reduction in viral load and 36 percent achieved an undetectable reading. In February, Trimeris’ Hopkins announced the latest results for the 46 HIVers in the study who had been taking T-20 for eight months. Although he did not clarify whether their viral loads were still undetectable, he did allow that their CD4s rose by 140.
So far, most T-20-takers have had mainly minor, routine side effects such as headache, fever and rash. But whether other adverse effects will accompany long-term use, as has happened with virtually every other antiretroviral, remains to be seen. Delaney, for one, is hopeful. “Given that T-20 does not interfere with DNA synthesis or any other proteins produced either by the virus or the body,” he says, “T-20 is largely a bystander, with limited ability to interact with other body processes.”
But on the drug resistance front, T-20 is no dazzler. While its “pattern” (the specific genetic mutations it causes in HIV) may be unique, thereby averting cross-resistance with other HAART meds, its “profile” -- the fact that HIV can develop resistance with just one or two mutations -- is no better than what’s already out there. Still, advocates like Gregg Gonsalves, policy director of the Treatment Action Group, applaud the new approach.
“T-20 and its cousins are a great step forward, especially for people with no other options,” he says. Delaney agrees, but predicts that T-20 will be expensive -- perhaps, he guesses, as much as a protease inhibitor. And other activists worry that Trimeris, concerned about increasing both injection burden and cost, may not be testing the drug in high-enough, best-working doses.
Chapter 5
In which Trimeris and T-20 enter the big leagues
The high cost and long delays built into the FDA approval process can drive a small company like Trimeris into the ground. Producing enough T-20 for testing and distribution has been a major hurdle. To make small quantities of T-20, researchers use a high-tech, 74-step process in which each peptide is built amino acid by amino acid (as if stringing pearls). According to M.C. King, PhD, Trimeris’ lead production researcher, this process is far from foolproof -- some sequences contain deletions or errors -- so each peptide must also be purified. Even after all that, King says, half of each yield is “junk.” To make larger quantities for clinical trials, Trimeris has come up with a streamlined process. To date, advocates credit Trimeris with being cooperative and fair in making trials of T-20 accessible to HIVers who most need new options. But blaming manufacturing costs, Trimeris has yet to provide the drug in the compassionate use or expanded-access programs that would reach many more HIVers.
As a drug enters big Phase III trials, a company must gear up to make large quantities. Trimeris opted for a route used by many small firms, joining forces with a behemoth flush with resources and infrastructure. Last July, Trimeris announced a deal with Roche, the Swiss drug giant that produces saquinavir and the PCR (polymerase chain reaction) viral load test. King says that plans for commercial T-20 manufacture are currently being worked out, as is a division of labor between the two companies.
Chapter 6
In which T-20 learns a painful lesson ... and marches on
Putting all your eggs in a single basket -- unless it contains the Golden Egg, which T-20 isn’t -- is not the best strategy for a small firm like Trimeris. As Gilead Science learned last year with its much-hyped adefovir, a nuke that looked good early on but crashed and burned in Phase III, only one out of 10 drugs with a shot at FDA approval panel ever wins the prize. So even as T-20 gets ready for its closeup, Trimeris researchers are already designing and testing second-generation candidates such as T-1249. Early studies look good: T-1249 appears to inhibit fusion as effectively as its cousin but is an advance on two fronts: It requires only once-a-day injections and works against HIV resistant to T-20.
Trimeris isn’t going to abandon T-20 in the home stretch, however. The drug is set to hit Phase III this summer. In November, Trimeris started its first trial of T-20 in kids. The drug won fast-track status in February 1999, as did T-1249, in May 1999. Bolognesi expects that Trimeris will have sufficient Phase III data -- proof that T-20 is safe and effective in a large number of HIVers for a year or more -- to file a New Drug Application with the FDA in late 2001. The anticipated launch for T-20 -- with its focus-group-tested brand name (to be announced) -- is set for early 2002. Only time will tell who, in chapter 7, lives happily ever after.
SHOOTING GALLERY
HIV and Its Three Enzyme Accomplices
Like most criminals, HIV needs sidekicks -- in this case, at least three enzymes that help it replicate genetically. Scientists are working on ways to knock these guys down, one by one.
T-20 blocks HIV from entering a cell. As shown in the illustration of HIV replication, once inside a cell, HIV sheds its protein coat and shoots out its genetic material. But this impotent RNA must then be converted into life-making DNA, and that’s where the reverse-transcriptase enzyme comes in. The first-approved anti-HIV drugs, reverse transcriptase inhibitors -- including both nucleoside analogs like AZT and non-nukes like nevirapine -- stop this enzyme from doing its job. But if the conversion is completed, the new DNA slips into the host cell’s nucleus and is shuffled into its chromosomes. Little is known about this process other than that it is carried out by the integrase enzyme -- accomplice No. 2, which scientists are also busy finding ways to foil.
Once HIV’s genetic material is integrated into the host cell’s chromosomes, it acts as a “blueprint” to direct the production of new HIV RNA. The RNA is then used to produce long protein chains, which must be cut up into smaller pieces before they can be assembled into new viruses. This snipping is accomplished by accomplice No. 3, the protease enzyme, which protease inhibitors such as indinavir, ritonavir and amprenavir were developed to tackle.
With a combo of drugs from different classes, it is possible to attack HIV on several lifecycle fronts at once.






Comments
Comments