Since 1994, POZ has featured countless people living with HIV in its pages. The subjects in these stories—everyone from everyday people who beat the odds to headline-grabbing advocates who spoke truth to power—have inspired readers throughout the country to take action, be resilient and remain optimistic even in dark times.
“POZ was a nexus for the PLHIV [people living with HIV] self-empowerment movement,” said founder Sean Strub in an interview for the 25th anniversary issue.
“I’m really proud of the people we featured in the magazine who were previously unknown to a large audience,” he said. “We consciously sought out people living with HIV doing great work and intentionally shined a spotlight on them as a strategy to amplify their voices and bring attention and resources to their work.”
The folks highlighted here represent just a tiny fraction of the personal stories POZ has shared over the years. However, they serve as examples of the many diverse groups affected by HIV, including long-term survivors, transgender people, women, Latinos and African Americans. These are their stories.
Fred Bingham
In 1981, when Bingham was diagnosed with AIDS, he changed his lifestyle. He experimented with herbs, stopped using street drugs and started taking Antabuse to combat his alcohol use disorder.
He also took massive amounts of antioxidants to restore sulfur-containing amino acids, and he learned everything he could about AIDS.
In 1987, AZT became the first drug approved for the treatment of HIV. However, its side effects were so terrible that many of those who took it stopped using it altogether. Like a lot of other people back then, Bingham relied instead on alternative treatments to fight the disease.
But in 1989, the professional horticulturist started using drugs and alcohol again and abandoned his health regimen. He experienced severe thrush and neuropathy, weight loss and stress. He was also diagnosed with dementia and wound up in the hospital with a CD4 count of 39.
Bingham requested AZT to help treat the neuropathy that was affecting his body (even though now we know AZT causes neuropathy) but soon stopped taking the medication because of its toxicity. That’s when he began to develop his own long-term intervention to manage his AIDS.
Once he got back on track, doctors were stunned to find that Bingham had reversed his condition. In 1994, Bingham, who then had a CD4 count of about 900, told POZ, “Technically, I’m in remission.” He also believed that “the one-drug, one-bug, one-million-dollar mentality [was] not serving people with HIV and AIDS very well.”
In response, Bingham founded Direct AIDS Alternative Information Resources, a nonprofit group that promoted self-empowered healing from HIV and its related illnesses. He operated it from his apartment. It was this do-it-yourself advocacy that the HIV community best remembered when he died in 2015.

Veronika Cauley
A Black HIV and transgender activist from San Francisco, Cauley was determined to make the health care system work for the transgender community.
Since the start of the epidemic, transgender people have had to fight to make their voices heard. In 1999, POZ wrote its first extensive story on this population. The article highlighted alarming HIV rates in San Francisco among transgender African-American women as well as discrimination and other barriers to care faced by people of trans experience.
The article also shone a light on Cauley, who began her transition in 1978 after leaving the Navy. She turned to sex work before becoming addicted to crack cocaine and getting arrested while living in New York City.
Cauley then fled to Indiana, where at the local Veterans Administration hospital she learned she had HIV—and doctors told her she had only five years to live. But Cauley continues to outlast her presumed expiration date.
After relocating to San Francisco, she lobbied to be appointed to the city’s veterans affairs (VA) commission to update HIV treatments in VA hospitals.
In 2018, Cauley—now Veronika Fimbres—hoped to become California’s first African-American transgender governor as a write-in candidate for the Green Party.
As she told POZ 25 years ago: “I have hope for the future—that they will find a cure, that transgenders will no longer be devalued. Because I think it’s the world’s diversity that makes it a better place.”

Dawn Averitt
When Averitt was diagnosed with HIV in 1988 at age 19, she didn’t think motherhood would be an option for her. She recalled coming across a statistic proclaiming that a pregnant woman with HIV had a 70% to 100% chance of transmitting the virus to her baby. But Averitt really wanted to be a mother.
Then, in 1996, the advent of effective antiretroviral (ARV) therapy for HIV meant that a mom with the virus no longer had to fear that her children would be orphaned in the near future. But was it safe to give birth? Averitt worried that the meds would be harmful to a fetus.
The reassuring answer to Averitt’s question came in the form of a 2001 study that revealed that taking ARVs during the first trimester of pregnancy did not increase the risk for birth defects. Further research showed that HIV treatment combined with good health care and bottle-feeding guaranteed that 99 out of every 100 women with HIV could become mothers with virtually no risk to their baby.
So Averitt decided to become a mother. In June 2002, she and her husband welcomed into the world an HIV-negative daughter, Maddy. Averitt and Maddy graced the cover of POZ’s December 2002 issue. That same year, Averitt founded The Well Project, a nonprofit that works to improve the lives of women living with HIV.
For long-term survivors, Averitt has this bit of advice: “Integrate HIV into your life. If you let HIV be a tumor, an invader, a growth, then the burden is too heavy. Once it is a part of your life (and not the sum total of your life), HIV becomes more manageable.”

The Reverend Stacy Latimer
Latimer, one of our 2007 cover subjects, is an HIV-positive minister and military vet who has relationships with men. The South Carolina native grew up in a religious family and had known from childhood that he was attracted to men. He kept this hidden throughout his adolescence, causing him much pain.
In 1987, while enlisted in the Army, Latimer learned he was HIV positive via a letter from the Red Cross about a blood donation he’d made. After sharing his diagnosis with a commanding officer, he was sent to Walter Reed National Military Medical Center in Bethesda, Maryland, which housed servicemen with HIV in a special ward.
Latimer spent so much of his time at the hospital comforting those who were critically ill and had been abandoned that patients assumed he was a volunteer.
However, Latimer still had his own demons to face. Struggling to process his HIV diagnosis, he turned to drugs and alcohol to help him cope. But Latimer says God came to him one night and showed him his purpose. He soon quit drugs and studied to become a religious leader.
Latimer went on to establish his own AIDS ministry and work closely with other pastors and faith leaders who have tested positive for the virus. Most important, he has traveled to Black churches and helped take on the difficult topic of HIV in their own congregations. He accomplishes this by sharing his own testimony and inspiring others to do the same.
“Our stories [of living with HIV], told with sincerity and integrity, carry the power to heal,” he told POZ. “They share wisdom, usher in peace and impart strength.”

Antonio Muñoz
Muñoz was diagnosed with HIV in 2008. At the time, he was about a year into his job at The Manhattan Club, a boutique hotel in New York City, and didn’t think he needed to disclose his status to his employer.
Between 2007 and 2011, Muñoz was such a model employee that he received the Exemplary Manager Award, several raises and positive evaluations from supervisors.
As his health declined, Muñoz’s doctor prescribed Sustiva, a drug known to cause drowsiness. This concerned Muñoz, who knew he could no longer work nights at the hotel. He asked for a shift change and submitted a doctor’s note explaining his health problems but was initially denied. Eventually, he was switched to a day shift.
But soon, the hotel put Muñoz back on the night shift. When he complained about it to human resources, his supervisors retaliated against him. Then, in 2011, after someone made an anonymous complaint about him, he was fired from his job.
Muñoz filed a civil lawsuit against The Manhattan Club for discrimination. In its counterargument, the hotel characterized Muñoz as a lazy complainer who didn’t do his job. Muñoz rejected that idea and said he was only trying to take care of his health.
In April 2013, a jury ruled in his favor in federal court. Muñoz was awarded $500,000 for wrongful termination as a result of HIV discrimination.
But it was never just about the money for Muñoz. It was about telling his story and being heard. As he told POZ readers in 2014: “You have to have determination to believe in yourself.”

Shana Cozad
A member of the Kiowa tribe in Oklahoma, Cozad has lived with HIV for more than two decades and is one of the first Native American women to speak openly about her HIV status. She is also one of nearly 4,000 American Indians and Alaska Natives estimated to be living with the virus.
While in college, Cozad contracted the virus from her boyfriend, who was only her second sexual partner. But it wasn’t until their breakup that he admitted to having AIDS. She didn’t believe him and assumed it was just a desperate ploy to keep them together.
A friend eventually convinced Cozad to get tested. It took three positive test results for Cozad to finally accept her diagnosis. Unfortunately, she also learned that her CD4 count was 189 and she was living with AIDS despite feeling fine.
Following her diagnosis, she turned to her tribal elders for help. They guided her through traditional healing ceremonies and overnight rites that lasted 12 to 15 hours. These ceremonies, Cozad said, helped release her anger at HIV.
Today, Cozad’s virus is undetectable. For this, she credits not only her antiretroviral medication but also her spiritual advisers, who taught her how to approach the disease and her body in a positive manner. In 2018, she told POZ, “HIV is a teacher for me. It has transformed my life. It has humbled me. I don’t feel cured, but I feel healed because I’m at peace with this disease.”

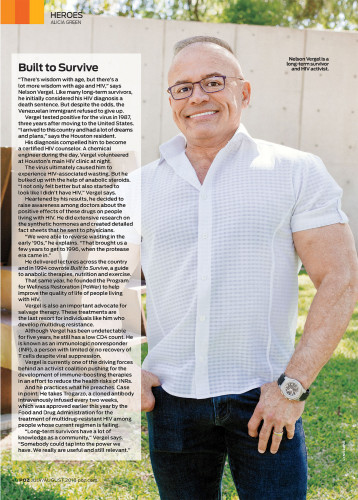
Nelson Vergel
When Vergel immigrated to the United States from Venezuela in 1984, he had a lot of dreams and plans. But they were all cut short when he tested positive for HIV just three years later. He considered his diagnosis a death sentence.
But Vergel never gave up. Instead, he told POZ in 2018, he became a certified HIV counselor who worked as a chemical engineer during the day and as a volunteer at a local clinic at night.
The virus caused Vergel to experience HIV-associated wasting, so he turned to anabolic steroids to help him regain weight. His success led him to advocate for these drugs for people living with HIV. In 1994, he cowrote Built to Survive, a guide to anabolic therapies, nutrition and exercise, and founded the Program for Wellness Restoration (PoWer) to help improve the quality of life for those with HIV.
When Vergel’s HIV became resistant to multiple drug therapies, he campaigned for salvage therapy—the development of entirely new meds—as a last resort for those like him. Luckily, he began to take Trogarzo, which was approved by the Food and Drug Administration in 2018 for the treatment of multidrug-resistant HIV among people whose current regimen is failing.
Since 2013, Vergel has had an undetectable viral load. But he still has a low CD4 count. This has prompted him to join an activist coalition that pushes for the development of immune-boosting therapies to reduce health risks for immunologic nonresponders, or people with limited or no recovery of CD4s despite viral suppression.
“Long-term survivors have a lot of knowledge as a community,” Vergel shared with POZ in 2018. “Somebody could tap into the power we have. We really are useful and still relevant.”






Comments
Comments