When will we have a COVID-19 vaccine?
Researchers have made good progress toward developing vaccines to prevent SARS-CoV-2, the new coronavirus that causes COVID-19. Experimental vaccine candidates have been shown to stimulate both the production of antibodies and T-cell immune responses against the virus in early studies. T-cell immunity is important because it may provide ongoing protection even if antibodies don’t last very long.
In November, interim results showed that three vaccines—from Pfizer and BioNTech, Moderna and the National Institutes of Health, and AstraZeneca and the University of Oxford—appear to reduce the risk of symptomatic COVID-19 by 90% or more. The first two use a novel mRNA approach never before used in an approved vaccine, while the third uses a weakened adenovirus vector. Other vaccines are in Phase III clinical trials—the last step before approval if they are shown to be safe and effective.
Although there is hope, experts predict that a vaccine will not be widely available for months. Once one or more vaccines are authorized, it will take time before they can be manufactured in large quantities and administered to all.
Istock
How do B cells and T cells fight disease?
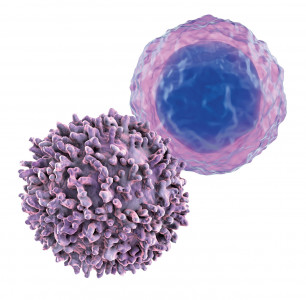
Several types of white blood cells play a role in immune responses against viruses and bacteria as well as cells that grow out of control and become cancerous.
Macrophages, neutrophils and other first responders provide the initial line of defense, attacking invaders and releasing chemical messengers called cytokines that cause inflammation. Natural killer cells destroy virus-infected cells and tumor cells.
B cells and T cells, two types of lymphocytes, are more specialized soldiers of the immune system. These cells recognize specific proteins called antigens on viruses, bacteria and cancer cells.
B cells produce antibodies, which bind to antigens and either block viruses and bacteria from entering cells (neutralizing antibodies) or trigger additional immune defenses.
The two main types of T cells are CD4 and CD8 cells.
CD4, or helper, T cells coordinate the immune response. These are the primary targets of HIV. As the virus destroys CD4 cells, people become susceptible to opportunistic infections and cancers. Suppressing the virus with antiretroviral therapy protects CD4 cells, and monitoring CD4 counts—along with viral load—can show whether treatment is working.
CD8, or killer, T cells (also known as cytotoxic T cells) directly attack invaders. Unfortunately, killer T cells are usually not able to keep HIV in check without antiretrovirals.
Vaccines mainly work by stimulating the production of antibodies, but they can promote T-cell activity too. Both antibody and T-cell responses play a role in fighting SARS-CoV-2, the new coronavirus that causes COVID-19. Checkpoint inhibitors, a type of immunotherapy, unleash T cells to fight cancer. Genetically engineered T cells, known as CAR-T therapy, are used to treat cancer and are under study for HIV.







Comments
Comments