 |
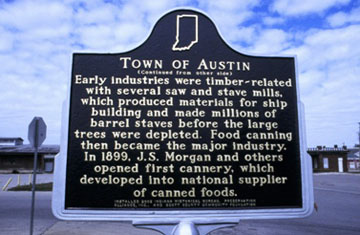
| Official marker in Austin, Indiana |
No AIDS activist could have predicted this story 25 years ago, when they first carried packets of sterile syringes and bleach kits into the streets of New York’s Lower East Side, setting up sidewalk swaps in defiance of the War on Drugs. But HIV has found a welcome home in rural America, where entire counties, from southern New York to northern Alabama, are increasingly caught in a socioeconomic death spiral, and where entire families are caught in the spiral of opiate addiction. Now needle exchanges may become, however improbably, as common a feature of small-town America as boarded-up storefronts and broken traffic lights.
Austin, in Scott County, Indiana, is a small town with a big addiction problem. Founded in 1853 as a rail stop between Louisville and Indianapolis, Austin’s relative isolation has made it a haven for drug traffickers on nearby Interstate 65, a major north-south thoroughfare. With the spike in prescription painkiller misuse over the past 15 years, these so-called "pillbillies" have put Austin on the map of opiate capitals.
Where the prostitutes roam.
And life gets worse every day.
Where the druggies run wild,
And the town is reviled.
But that’s just the Austin way."
— a comment on "The Eyes of the World Are on Austin"
forum on the Topix.com website.
Of Austin’s 4,225 residents, as many as 10 percent may inject opiates on a daily basis. The other 90 percent do not escape addiction’s fallout, however. “Because of the size of the community, everybody knows someone involved: a family member or a friend or somebody who has been affected by this,” the town’s chief of police, Donald Spicer, told the BBC. His wife, Linda Richie Spicer, who is running for mayor, told Al Jazeera America, “The drug problem is near and dear to my heart — I just buried my niece in February.”
Addiction is a disease of the emotionally and economically depressed. Austin has a 9 percent unemployment rate and a $16,000 per capita income. It has 35 churches and one doctor. Yet only when Austin’s drug-using population became a public health emergency — and a national media story — did the town’s woes merit the attention of state officials.
The HIV outbreak was first detected in November 2014, when three people in Scott County tested positive for the virus. (Its annual number of new cases had previously never exceeded five.) On February 25, the Indiana State Health Department made its first announcement, reporting 30 new HIV infections since mid-December. Two days later, the number had grown to 37. "This is the first outbreak of HIV among drug users injecting an oral opioid in a rural community in recent years, [and] one of the worst outbreaks among IV users in the past two decades," said Jonathan Mermin, MD, MPH, who heads the Centers for Disease Control and Prevention’s (CDC) center for HIV/AIDS prevention.
By March 20, there were 68 infections. The next day, two CDC epidemiologists flew to Austin to begin contact tracing. Austin’s injection drug users (IDUs) shoot up, on average, from four to 15 times a day; the number of people at a single “injection event” may be as high as six. “Sometimes two, even three, generations will all be IV drug users,” the Scott County public health nurse, Brittany Combs, RN, told Politico. “That’s one of the ways HIV spread so quickly: [People will say,] ’I only share [needles] with my family.’ They trusted them and shared needles with them. It’s pretty shocking.”
On March 26, Indiana’s Republican governor, Mike Pence, signed an executive order overriding the state law criminalizing syringe swaps. A staunch anti-drug warrior, Pence said that he would “make an exception” and authorize a “limited and focused” 30-day needle exchange. “I’m going to put the lives of the people of Indiana first.... It’s a commitment to law and order, but it’s a commitment to compassion,” he said.
The announcement came one day after the Kentucky state legislature passed an “anti-heroin” law legalizing syringe swaps in an effort to avert its own IV-drug-related HIV crisis.
The harm reduction movement is having a moment. “Conservative, rural states adopting syringe programs is a game-changer,” said Bill Piper, director of national affairs for the Drug Policy Alliance. “There’s an opportunity here for the U.S. to join the rest of the developed world in making sterile syringes widely available to stamp out deadly diseases.”
Yet Pence’s decision was only the promise of progress. Whether syringe swaps, which have their U.S. roots in urban, primarily African-American and Latino, drug-using neighborhoods, could be successfully transplanted to a rural county like Austin, which is 92 percent Republican and 99 percent white, was uncertain. The commitment to law and order and the commitment to compassion are often in competition, and their differences can be reconciled much easier at the level of rhetoric than in reality.
By March 27, the number of new HIV infections had grown to 81.
 |
| Indiana Governor Mike Pence |
From the first, officials took pains to insist that Austin was the proverbial canary in the coal mine. “There is nothing that makes Scott County different from any other rural county in America,” Indiana deputy health commissioner Jennifer Walthall, MD, MPH, said at one of the media updates held at Austin City Hall every week during the crisis. “There is an opiate epidemic across the United States. The sharing of needles for injection drug use is not limited to Scott County. What brought our attention to the absolute imperative need for comprehensive services was the combination of HIV, hepatitis C and injection drug use in one setting.”
A pernicious set of factors makes rural America vulnerable to the opiate epidemic. As traditional industries like manufacturing depart, the local economy tanks. Businesses go bust, tax revenues plunge, schools and hospitals close, public services end. Facing bleak employment prospects, a community’s more resourceful members — especially the young — move away, leaving behind an aging workforce. Add the overprescribing of opioid painkillers, and the community’s less resourceful children can find a chemical escape from poverty in the family medicine cabinet.
They can also find a commercial escape. “A lot of it starts out legal, grandma has it in the counter, she’s been given the medicine for whatever reason,” Donald Spicer told WDRB News, the local Fox affiliate. “Maybe the grandson says, ’Hey grandma, you draw $800 a month, you can get $120 or $140 a pill out of this medicine you have.’ And you know, that becomes pretty entertaining to people.”
A recent crackdown on pill mills in Florida and other Southern states, coupled with new crush-proof formulations, has caused many users to switch to heroin. Yet in Scott County, addicts have been able to access extended-release Opana (oxymorphone) — specifically the 40 milligram tablets that are not crush proof — thanks mainly to its close proximity to I-65. When cooked and liquefied, a single pill yields eight doses, ideal for sharing. The high is faster, harder, and briefer than other opiates, increasing its addictiveness. “There ain’t nothing like Opana,” HIV-positive Austin native Kevin Polly told Al Jazeera America. “It’s sick, but true.”
Many states, including Indiana, have also toughened their prescription drug laws, making it a felony to be caught with a hypodermic or other injecting materials. “We had to use the same needle over and over again because you just couldn’t find them,” Polly said. “It was nothing to share a needle. As long as we got the Opana in us, it didn’t matter.”
William Cooke, MD, opened Foundations Family Medicine (FFM) in Austin in 2004. Cooke, who is in his late 30s, has long black hair and a scruffy beard that is less a style statement than the result of his long hours at FFM and a second job at the Scott Memorial Hospital ER. His blue scrubs, open face and slightly nasal voice became a familiar feature in the media coverage of the outbreak as he explained, over and over, how it was allowed to happen.
“We saw this coming, for sure,” he told the Louisville Courier-Journal. “But I never expected it to be like this. It’s spreading and it’s going to spread. It’s a demonstration of what happens when we ignore a demographic group.”
Over the past 11 years, Cooke has built up a practice of over 12,000 patients. He has taken the pulse of his community’s substance-misuse problem, watching helplessly as addicted patients disappeared from care even when he dropped his fees to $20 or less. (One of his nurses has lost five relatives to overdose and other addiction-related complications.)
Cooke said that he “repeatedly asked for help” from county and state health officials, to no avail. “Everybody would agree it’s a problem, everybody would agree something needed to be done, but everybody was busy with other priorities.”
Indiana invests $13.08 per capita annually for public health. The CDC and HRSA spend less per capita in Indiana than in any other state, according to Indiana University’s Rural Center for AIDS/STD Prevention (RCAP). Scott County has no budget for HIV or hepatitis C virus (HCV) testing. As for substance use treatment, there are only 23 programs in all of southern Indiana.
With the advent of the Great Recession and the Obama presidency, hard-right Republicans took over state governments and proceeded to slash public funding. State and county health departments were prime targets. “Rural public health is leaner than the urban settings, so cuts disproportionately impact them,” Georges Benjamin, the director of the American Public Health Association, told USA Today.
Gov. Pence initially rejected Affordable Care Act funds to expand HIP, the state’s version of Medicaid. In January, he reversed that decision. When 11 of the 120 prisoners in the Scott County Jail tested HIV positive in March, Sheriff Dan McClain denied them treatment because his budget did not contain an annual $20,000 for a prisoner’s HIV meds. “That’s a discussion I’ve had with the governor,” he told The New York Times. “Once we get that support, we’ll screen whoever comes through our doors, medicate them, educate them and eventually refer them over to Dr. Cooke.”
More than once Cooke came close to quitting and leaving town. Then the storm hit, and he was at its center.
On March 25, he announced that he would open a weekly free HIV clinic at his FFM offices on March 31. His nurses would do HIV testing. He arranged for two HIV specialists associated with Indiana University Health’s health care system to treat people who test positive. The town’s two pharmacies were stocking up on HIV drugs. The Los Angeles-based AIDS Healthcare Foundation (AHF) was asked to provide mobile HIV testing.
“I’m doing this on faith,” Cooke told NBC News. “Yes, we need to get paid as a clinic [to offer] all of this. But that’s not the No. 1 concern now. The No. 1 concern is getting these people into treatment...[and to] reduce this viral load that’s just running rampant through the community.”
For some people in Austin, however, the No. 1 concern was the presence of the HIV clinic itself. As word got around, many of his regular patients canceled their appointments. “We have been yelled at, cussed at and told off because of what we are doing, getting harassing and threatening phone calls,” his office manager said. (Cooke did not respond to POZ’s request for an interview.)
 |
| Sterile syringes stir controversy |
On March 31, Dan Bigg parked a 16-foot rental truck in front of Cooke’s offices on Main Street. The cofounder and director of the Chicago Recovery Alliance (CRA), Bigg began unloading box after box of sterile syringes and other injection drug supplies with three fellow harm-reduction workers. CRA had been asked by the state health department to lend its expertise to Austin’s effort to set up an exchange. The group has a decades-long history of training people to organize successful exchanges, even in neighborhoods rife with violent drug crime.
The syringe giveaway was up and running soon after the HIV clinic opened at 9 a.m. “This was an emergency and we treated it as such,” Bigg tells POZ. “We went out into the neighborhood to make contact with as many drug users as possible.” Given that the program had only been authorized for 30 days, CRA did aggressive peer distribution, enlisting folks who were using the exchange to supply those who were not. On the first day CRA was able to reach about 60 Austin IDUs.
It is in the nature of activists to test the limits of a given situation. Yet the idea of drug users carrying boxes of syringes home with them did not exactly play in the police department. Austin residents had long been up in arms about the proliferation of dirty needles in gutters and parking lots, front lawns and playgrounds. Far from viewing CRA as experts sent to show how it is done, Donald Spicer dismissed them as outside agitators advancing their own political agenda. “Peer distribution,” to his mind, was a felony, and he threatened Bigg with arrest.
On April 3, nine police officers showed up at Kevin Polly’s door. “I had received 1,500 syringes [from Bigg] that I was giving out to people in the community that are afraid to go get help [because of] repercussions like this,” Polly said. “And I was down to about 130. They confiscated those from me.” A woman in the house was jailed when a single needle was found in her room, Polly said. (The woman was selling Opana, according to Spicer.)
“The whole situation was very disturbing,” Bigg says. “The Scott County health department acted like they didn’t care about the needle exchange. It almost seemed like they wanted it to fail.”
Under this cloud of mistrust, the Austin needle exchange opened on April 4 in a nondescript one-story building in an industrial park on the outskirts of town. Officially billed the “One Stop Shop,” it offered sterile syringes, HIV testing, condoms, immunizations for tetanus and hepatitis A and B, HIP 2.0 enrollment, substance-use treatment referrals — in short, everything Cooke could have dreamed of, plus a door-to-door shuttle bus driven by a church volunteer. Some $2 million in state funding was falling from the sky. There was one problem, however: After four days, a total of four people had come to the One Stop Shop. Meantime, the number of people who had tested HIV positive had grown to 106.
Unlike CRA’s giveaway, to get a clean needle from the One Stop Shop, you had to first register for a card and return a used needle. Neither policy inspired trust in drug users. Even though you did not have to give your full name (just your birth date, sex and the first two letters of your first and last names), drug users already feared being arrested for carrying needles. Now they feared being arrested for carrying the cards. And who wanted to be seen walking into the One Stop Shop in broad daylight to get tested for HIV?
After CRA returned to Chicago, Bigg said, “I heard that they were compromising people’s anonymity and collaborating with the police.”
Officials denied this. “We don’t report these people, we don’t track these people. We are simply trying to get them to stop using dirty needles,” Brittany Combs told the county paper, the Giveaway.
“We are not arresting anyone coming to the center for clean needles. That isn’t the goal of this program,” said Donald Spicer, who blamed CRA for handing out so many syringes that no one needed to use the program.
Spicer may not have wanted the exchange to fail, but he made little effort to conceal his ambivalence. “If [the NEP] is going to save lives, I have to support what theyre telling me will work, because they know more about it than I do,” he told Al Jazeera America. “[But] from the law enforcement side of it, I can’t support it, because we’re not able to do what we need to do. We’re giving people things to use drugs with.”
In an HIV outbreak, enforcing laws that criminalize IDUs drives them underground, undermining public health measures to engage them. Harm reduction workers generally spend months laying the foundation for a needle exchange, meeting with health officials, local law enforcement, business owners and the community in general, working to win their trust. “This was a response to a crisis. The people who are doing it had no prior experience. To some extent, it was sprung on them,” Daniel Raymond, the policy director of the New York–based Harm Reduction Coalition, tells POZ. “Local law enforcement was being asked to do a 180-degree turn in a matter of days. But building trust takes time.”
 |
| 1990 Health Policy Advisory Council bulletin |
On April 20, Gov. Pence extended the Austin needle exchange for an additional 30 days. By then, 130 people had tested HIV positive. Indiana state health commissioner Jerome Adams, MD, MPH, a Pence appointee, was careful to say that needle exchanges were a viable measure only if they succeeded in getting people to stop using drugs. “People just want to say, ’OK, needles for everyone, everywhere.’ It’s only going to work if it allows us to connect people to the resources they need to get clean...and get their infectious diseases treated,” he told The New York Times.
Clark County public health director Kenneth Burke, MD, who is in charge of HIV testing in southeastern Indiana, broke ranks with his boss. “Some of these people are going to abuse IV drugs until they die,” he said. “But I don’t think there’s any question that you decrease the risk of infection by allowing them to use clean needles.”
These opposing positions frame the classic debate about exchanges and, ultimately, about the value of the life of a drug user. For Burke, that life has an unconditional value; for Adams, drug users are a disposable population.
Opponents of needle exchange have always argued that they increase drug use. For two decades, studies have shown that this is false; they increase safer drug use. Yet proponents have always argued that they do more than that.
“The terms ’needle exchange’ and ’needle distribution’ do not do justice to the concepts that they try to name. The words refer to only a small part of the event that needle exchange is,” wrote Rod Sorge in 1990. Sorge, who co-founded ACT UP’s needle exchange committee and the Harm Reduction Coalition, died of AIDS complications at age 30 in 1999. “It is the interaction between the giver and receiver of the needle that is the significant component of needle exchange, especially when encounters are repeated. And trust — maybe even friendship — is established.”
While an exchange is a “bridge” for users to get treatment for HIV, HCV and addiction — and studies show that people who use syringe swaps seek treatment at a rate five times greater than those who do not use them — the goal is to keep the user alive. Full stop.
Austin’s drug users live mainly on the north side of town. The northern end is the poor, “bad” part of town, and always has been. Its history reveals how entrenched the causes of the current crisis are and therefore how radical the fixes must be.
Austin was, for most of the 20th century, a company town; the workers had an essentially feudal relationship to their employer, the Morgan Packing Company, founded in 1899. As the nationwide demand for canned food exploded after World War I, Morgan built an empire of factories across southeastern Indiana. It filled the factories with unskilled labor from Appalachia, resettling a dirt-poor population on Austin’s north side.
Morgan built wooden bungalows to house its workers, a store to feed and clothe them, even a hall downtown for them to dance and get drunk in on Saturday nights. The company recouped the workers’ wages in the form of rent and other bills, ensuring itself a more or less captive labor force for generations. The town of Austin never fully assimilated these families, and they remained displaced Appalachians who are still today derided as “hillbillies.”
With the decline of the canning industry, the company, now called Morgan Foods, shut down all its factories except the Austin location. But because many descendants of the original Appalachians have substance-misuse problems or cannot pass criminal background checks, Morgan now recruits mainly outside of the town. “I think if the government is wanting to help us users, they need to put a clinic here or more vocational programs or even letting convicted felons get a job. Because I’m a convicted felon, so it’s hard for me to get a job,” Austin resident Tiffany Prater told NWI.com.
If Austin had long bristled under its notoriety as an opiate haven, it now brayed under its new title as the Town With the HIV Outbreak.
“Throughout the nation, American citizens are reading about this ’rural Indiana town’ that is the epicenter of one of the largest HIV epidemics in our nation’s history,” began a column by Austin High School senior Josh Davidson in a “Special [HIV] Crisis” edition of the student newspaper, The Eagle, published on April 10. “As I am writing this, I am certain that across the world, the populace of our city is being labeled as ’poverty stricken’ and uneducated. I strongly disagree with the description because I have not only seen, I have experienced the lighter side of Austin, and I think it is time that we take a stand. I refuse to allow my community to be labeled as a result of the actions of a few people.”
In story after story after story, the media focused on the signs of disrepair and squalor on the north side of town: “dilapidated [houses] with peeling paint and boarded-up windows,” “yards dotted with old cars, broken furniture and trash,” “tiny Pentecostal churches and Confederate flags,” “the smell of meth in the air.” Most houses were not drug houses, however, and many had quite different signs. “No loitering and prostituting in front of or around these premises. Violators will be prosecuted,” read a hand-written cardboard sign on Tammy Breeding’s porch, and: “Warning: Security Cameras in Use.”
“I’m fed up with having to run the drug users off my property,” Breeding, a single mother and Austin native, told Kaiser Health News. “They’re making drug deals at the corner, prostitutes are getting picked up in front of my house, and my kids are seeing it all.” She told WDRB, “They’re out here driving high, they’re on mopeds high, they’re walking high — it’s like the walking dead out here at nighttime.” (Breeding did not respond to POZ’s request for an interview.)
In the news clip, Breeding stands on her front lawn, her arms crossed and a handgun in a holster on her side — a mama grizzly taking a stand. “The people in this town are scared to say anything because of the retaliation from the drug users. I’ve gotten threatened four or five times. One told me I need to get out of town,” she says. "If they want to [start] something, Mr. Ruger will meet them in the end. And I don’t miss my target." She pats her gun.
When asked about the needle exchange, Breeding says, “The drug users don’t need a needle exchange. What they need is treatment.” Yet Austin has no drug treatment. If the town is rich in anything, it is churches, and in April, a coalition of churches countywide organized a weekly “prayer walk” of between 100 and 200 people, complete with a tape of Christian music and a live horn. In the general absence of other resources to deal with addiction, this spiritual intervention is a last resort. They walk, and as they walk, they call out, “Jesus loves you,” to drug users. They form a circle in front of drug houses and, holding hands, pray for the “healing of souls.” They knock on doors, inviting drug users to join them.
 |
| Jeanne White-Ginder |
Where there is HIV there will be HIV stigma, and Austin is no exception. The town already had something of a siege mentality. “These people dealing with these drugs are so bad, they just as soon to kill you as look at you,” Donnie Estep told PBS News. (The Scott County health department deleted the post on its Facebook page announcing the needle exchange because of the high volume of vituperative comments.) As the number of new HIV diagnoses mounted, classically wayward fears of contagion gathered force.
Mothers feared that their kids would get HIV from the dirty needles in the playgrounds. Sports teams from other high schools feared that the balls used by Austin players had HIV in them. Some people at high risk were not getting tested because they feared that HIV would be a death sentence; others who tested positive feared that they themselves were toxic. “There are still a significant proportion of people in Austin who have biases about HIV and are contributing to the stigma and subsequent fear,” Diane Janowicz, MD, one of the two infectious disease specialists in Cooke’s clinic, told the Louisville Courier-Journal. “I have to reassure them — if your grandkid wants a sip of your drink, you can share it. It’s OK to eat at the same table.”
Despite the many stacks of “HIV Facts” leaflets around town, a rumor started that a security camera caught three people injecting meat with HIV-infected blood at the local Walmart. It was about then that the Indiana Department of Health had the inspired idea to invite Jeanne White-Grinder to tell Austin about “the legacy of Ryan White.”
“My job was to tell Ryan’s and my story, and through that to help these people who were so scared understand the stigma around AIDS,” White-Grinder tells POZ of her visit in May, when between 300 and 400 people filled the Austin High School auditorium to hear her. White-Grinder is a fellow Hoosier, and it was a Russiaville, Indiana, middle school that had banned her son, Ryan, as a public health danger when the 13-year-old’s AIDS diagnosis became known in 1985. The protracted legal battle that pitted the White family, supported by the Indiana health department, against the good people of Russiaville was a parable unlikely to escape the good people of Austin in 2015.
“There was some school bullying going on — certain students’ photos posted on Facebook saying they had AIDS — and I especially wanted to address that,” she said. Jeanne and Ryan White won their battle against Western Middle School, but it was a pyrrhic victory. Ryan attended eighth grade, and was bullied, ostracized, segregated, and otherwise humiliated by his fellow students, their parents and school employees. When a bullet was shot through a window of their house, the family was left with no option but flight. In 1990, Ryan White died, the world’s most famous and beloved face of AIDS, one month short of his high school graduation.
“Austin just shows the level of panic we still have about AIDS in many parts of this country,” White-Grinder says.
By April 21, 135 people had tested positive for HIV. AHF’s HIV testing van had become a regular presence; churches and convenience stores let it park in their lots. A mobile needle exchange was also making the rounds, thanks to Brittany Combs, who had got her hands on a white SUV, filled the back with hundreds of sterile syringes and hit the streets. Wearing a blue “Health Dept. Staff” T-shirt, she was forthright in her advocacy of the exchange and enthusiastic about her interactions with its users, even taking needles door to door. The health department recognized the failure of the strict one-for-one needle exchange policy and increased the handout to a week’s supply. (This is defined as the number of times an individual injects drugs in a day times seven, with a maximum of 140.)
“We give them enough needles to last a week because we want them to keep coming in every week. Every single time somebody comes in, they get substance abuse [and] harm reduction education,” Combs told PBS. “And that’s our goal — to get them to come back — and then they trust you more.”
This strategy, combined with what Combs called “mission work,” began showing some success. Between April 25 and May 7, the number of people who got clean syringes more than doubled, to a total of 250. By May 14, it had grown to 326, and more than half were new visits.
Combs took to distributing new syringes in a striking style that stripped the act of stigma, leaning out the window of the van and shouting, “Anybody need clean needles today?” and entering homes to ferret out recalcitrant folks. “Yesterday, we had people running after us, waving us down,” she told NPR at the beginning of June.
The nurse cannot deploy aggressive distribution without the support of Austin police chief Donald Spicer, who has apparently come around. “It was against the law for such a long time to possess a needle, so we’ve had to adapt on the fly and approach it in a different method. But our first concern is their health and the second is to try to enforce the law,” he told Canada’s CBC News.
Yet conflict remains over the enforcement of anti-paraphernalia laws: While the county prosecutor said that the governor’s executive order temporarily blocked all arrests, the sheriff told The New York Times, “If they’ve got one needle and they’re not in the program, they’re going to jail,” acknowledging that this was intended to intimidate drug users into enrolling.
The most recent data (June 10) reported that over the eight weeks since the One Stop Shop (and the mobile exchange) began operating, 25,187 used syringes had been brought in (at least one-quarter by police and community pickup), and 25,739 sterile syringes had been given out.
“In four hours of operation we distributed 50,000 syringes,” CRA’s Dan Bigg tells POZ. “In nine weeks of operation they distributed 25,000 syringes.”
Bigg’s calculus raises a vexed ethical dilemma: Getting more clean needles into more hands more quickly would almost certainly have prevented more infections, but the likely crackdown from local law enforcement might have sabotaged the exchange and further criminalized drug users. Like it or not, Austin had to create a needle exchange in its own image in order to achieve sustainability, which is an ongoing negotiation of trust with the entire community, according to the Harm Reduction Coalition’s Daniel Raymond. “The fact that after six weeks they have more than 300 people participating speaks for itself. They are making it work,” he tells POZ. “They have the best needle exchange that works for them.” Without the town’s support, the exchange will become vulnerable, “and that makes the very people the exchange is there to serve vulnerable too.”
 |
| Opana tablets |
"We feel that we are starting to get a handle on where we are in the outbreak," deputy health commissioner Jennifer Walthall said at the May 7 weekly update. “We have seen a drop-off in new contacts.” With each person who tested positive giving, on average, the names of nine partners who were at risk, it took only a few weeks for the CDC epidemiologists to inform a sufficient proportion of needle-sharers to break the HIV chain.
Not everyone is eager to get tested, however. In an interview in the “Special HIV Crisis” issue of the high school newspaper, a young woman who described herself as a sex-worker and addicted to Opana voiced her fear of the potential criminal ramifications involved in knowing that she has HIV. “If you are tested positive as a prostitute and then caught with man by a cop, they can get you for first-degree murder. Therefore, no woman is getting tested in the business. Of course I am scared of getting HIV, but I have to have money in order to survive, so I am being more cautious.” (As of June 10, 10 women who tested positive self-identified as “former prostitutes.”)
And on May 11, “we all got the news that an 18-year-old pregnant girl had died of ’full-blown’ AIDS,” Garith Fulham, AHF’s director of public policy and advocacy for Indiana and Ohio, tells POZ. “That was a wake-up call. Since when does that happen in the developed world?”
Yet even as the number of weekly new seropositive test results continued to rise — 150 (May 7), 158 (May 19), 162 (May 26), 169 (June 10), 170 (June 17) — the rate has slowed. (At press time, there were no reports of new cases.) Now attention focuses on the staggering challenge that this staggering rate of HIV will pose to the town for decades to come. According to the CDC, 491 people are entangled in the outbreak; of them, 408, or 83 percent, have been located; 387 agreed to be tested for HIV; and 169, or 40 percent, tested positive (85 percent also have HCV). Officials said that 21 refused to be tested. These newly infected people range in age from 18 to 57, with the average age 35. By comparison, during the worst days of the AIDS crisis, HIV infection rates among IDUs in New York City were between 50 and 60 percent.
On May 21, two days before the needle exchange’s expiration, Indiana state health commissioner Jerome Adams approved Austin’s request for a one-year extension of the program through May 24, 2016. At the videotaped public hearing in Austin City Hall, no one spoke up for or against it. The absence of pitchforks and torches does not prove widespread acceptance; at best, local officials see the necessity of the exchange’s sustainability.
Yet it is this very sustainability that remains in question. With the crisis putatively under control, the state health department announced on June 17 that it was pulling out of Scott County. “This is a transition to more local control, more local empowerment. But the state will remain partners with Scott County,” state health commissioner Adams said.
“Local empowerment” is a euphemism for “no public funding.” From Scott County’s perspective, the state seemed to be pulling the plug on the entire HIV intervention. Funding for the One Stop Shop ended on June 30, leaving the county scrambling to find cheaper digs: It cannot afford the $10,000 monthly rent. Lacking a budget to even pay for HIV testing and sterile syringes, the county was scrambling, period.
There were other problems too. In mid-May, the Indiana University HIV specialists who were treating newly diagnosed patients abruptly left Cooke’s practice in protest after the doctor signed a contract with the AIDS Healthcare Foundation. The focus of the rift, which disrupted patient care, was AHF’s president, Michael Weinstein, who has alienated many HIV advocates and public health officials with his campaign against PrEP, including allegedly using the agency’s clout to delay rollout of the state-of-the-art treatment-as-prevention measure in Los Angeles. On top of that, in April, three former AHF managers filed a lawsuit alleging that the agency engaged in a $20 million scam in 12 states to bilk Medicare and Medicaid by paying employees bonuses to refer patients to AHF’s own clinics and pharmacies.
“This process has not been easy. There have been concerns from Indiana University Health about the past reputation of the AIDS Healthcare Foundation and some activities that have occurred in the past,” deputy health commissioner Walthall told WISHTV.com on June 17. Announcing that the state health department would provide Scott County with the services of two additional nurses (one for the jails), two HIV care coordinators, one disease investigation specialist and one HIV/HCV tester, Walthall also made a point of emphasizing that PrEP will be available.
As for substance abuse treatment, a small outpatient program will open near Austin. Opiate addiction is a beast to kick, with rates of first relapse around 90 percent. At best, HIV-positive drug users may be given priority to access over those who have not seroconverted. And while many studies show that methadone maintenance therapy works best, the medication remains widely stigmatized as “one drug substituted for another” and is grossly underutilized, despite its recommendation by the NIH. If you live in Scott County, you have to drive 30 miles to Louisville to find the nearest methadone clinic.
Gov. Pence signed a bill on April 30 allowing all Indiana counties to establish one-year needle exchange programs for IV drug-related public health emergencies. The new law contains no new funding for such programs. What it does contain, however, is an elaborate legal framework — critics call it red tape — that makes approval of a new exchange contingent on a county proving that an HIV epidemic already exists. “[The requirement to] first demonstrate the existence of a public health emergency...ensures that they can only respond to, rather than prevent, new outbreaks,” the New England Journal of Medicine reported on June 24. Not surprisingly, few rural counties have the budget for widespread HIV and HCV testing of a hard-to-reach population of injection drug users, not to mention stepping up surveillance of arrest records, overdose deaths, opioid sales and other data. Indiana’s annual $13.08 per capita for public health bankrolls HIP 2.0 (state Medicaid), with little left over for the balance of health care. Lacking new funding, the law offers rural towns the opportunity to close the barn door after the horse has bolted.
“I thought the HIV outbreak in Austin might cause a groundswell around increasing our state’s investment in public health, but no one took up that cause,” Beth Meyerson, assistant professor at the Indiana University School of Public Health and the co-director of RCAP, tells POZ. “The good news is that the need for exchanges will be all too easy to demonstrate once testing is available.” RCAP’s Project Cultivate, which works with communities interested in a syringe swap, will launch a crowdsourcing effort in July to raise private funding to buy HIV and HCV testing kits. Lifting the ban on federal funding for exchanges could help states foot the bill, but Congress shows no signs of heeding the lesson of Austin. For the first time, however, HIV is a looming crisis in blue-collar communities in dark red states whose conservative lawmakers cherish their “tough on crime” credentials. While many elected officials may view the people at risk as smack-crazed junkies, this population is almost entirely white, and that may make a difference.
Advocates will continue to make a cost-effectiveness case that is attracting growing bipartisan support for other drug law reform. A single sterile syringe costs $0.97. An entire needle exchange program spends about $10,000 for each infection it prevents. By contrast, each person in Austin who is infected with HIV due to the lack of a clean needle will accrue about $1 million in lifetime HIV treatment and care costs (not including around $100,000 for a single course of HCV treatment). The U.S. taxpayer will foot the bill, through Medicaid, ADAP, the Ryan White CARE Act and other public funding. The sustainability of this safety net over decades is far from secure, however. “The politics of trying to prevent diseases among stigmatized groups are pretty rough,” Don Des Jarlais, director of research for the chemical dependency institute at Beth Israel Medical Center in New York City, told Politico. “It’s probably going to take more cases of HIV among rural Americans before we get the federal ban change.”
Therefore it is a question of where rather than whether another HIV outbreak will occur. Madison County, in central Indiana, has already gotten state approval to launch a syringe swap, while Jefferson and Clark counties, both of which border Scott County, have declared public health emergencies, and seven other Indiana counties “are making moves to do the same,” according to RCAP’s Meyerson. This development met with some dismay from the state health commissioner, who said, “Just because we find that there’s an epidemic in an area, doesn’t automatically mean a needle exchange needs to be part of that response.”
Louisville, Kentucky, opened its first needle exchange on June 10, with Lexington’s set to come online by Labor Day. Farther afield, the coalfields of West Virginia seem a shoe-in, thanks to the state’s No. 1 national ranking in overdose deaths and No. 2 in new HCV cases, but needle exchange remains illegal in that state.
 |
| “Warning HIV Outbreak” sign |
As Austin illustrates, the entrance of a single case of HIV into an isolated, insular village of drug users can spark a wildfire. Genetic testing of HIV samples from 72, or close to half, of those who tested positive since mid-December showed that 69 were identical, indicating that the virus was likely introduced between January and June of 2014. “Scott County is on [Interstate 65], a major trucking route,” Des Jarlais told Politico. “No one has tracked down how the virus got into Scott County, but that’s how it got there.”
That may explain why two big digital construction signs on I-65 north and south of Scott County were programmed to read “Danger HIV Outbreak” on May 1. I-65 is a 14-lane freeway that runs from Gary, Indiana, to Mobile, Alabama; Austin’s sex workers, many of whom are also drug users, often work the local truck stops. To many motorists, the state traffic department’s signs undoubtedly read as a warning to avoid the area, as if Scott County were a dump for hazardous waste. To many people with HIV, the signs read as a warning that they were viewed as hazardous waste. The electronic message boards were up for more than a month before protests came in June from HIV activists, including Josh Robbins. The state health department scrambled to get the transportation department to unplug the signs. “[This] was an accident and not intentional. However, that doesn’t remedy the fact that many of the people who live with HIV every day were put in a very difficult situation and we apologize deeply for that,” Jennifer Walthall told WISHTV.com.
“Danger HIV Outbreak” may well have been one clueless transportation department worker’s idea of HIV prevention. The truly dangerous idea is that preventing HIV outbreaks in these hollowed-out, addiction-riddled communities can be done on the cheap, with only sterile syringes, digital construction signs and church prayer walks.
Austin’s opiate addiction problem spans three generations and derives from seemingly intractable socioeconomic dysfunction. “The potential for continued transmission will be there for a decade or more,” Des Jarlais told The Associated Press. According to the most recent data (June 17), only 11 people, or 6 percent of the entire HIV positive population in Austin, were on treatment and had an undetectable viral load. On July 1, Scott County health officials announced that the needle exchange was open for business in a new, more affordable location. It is now next door to the police department.
 |
| Walter Armstrong |
Walter Armstrong is a former editor-in-chief of POZ magazine, the former deputy editor at The Fix and Substance.com (both drug-related magazines), and a freelance writer.







1 Comment
1 Comment