October 15th was National Latinx AIDS Awareness Day. It’s theme—“Living with HIV or not … we’re fighting this together”—exhorts us to promote solidarity, expand access to prevention and treatment, and address the stigma that weighs heavily on HIV in the Latinx community. The theme recognizes the continued social and structural barriers to eradicating HIV in the United States, where racial, ethnic and geographic inequalities remain obstacles to progress.
The Latinx population is disproportionately impacted by HIV. Despite comprising only 18% of the U.S. population, roughly 26% of people diagnosed with HIV in 2017 were Latinx. The disparity is also evident among Latino men who have sex with men (MSM), who comprised 20% of all new HIV diagnoses in 2017. Despite decreases in new HIV cases among most at-risk communities across racial and ethnic groups between 2010 and 2016, HIV diagnoses among Latino MSM rose by 18% overall and by 34% among young (ages 25 to 34) Latino MSM.
Increased attention has been given to the national HIV response since President Trump announced “Ending the HIV Epidemic: A Plan for America” in his 2019 State of the Union address. The initiative (EHE) aims to reduce new HIV cases in the United States by 75% within the next five years by initially focusing efforts on 50 jurisdictions with the highest HIV burden and seven states with substantial rates of HIV in rural areas.
Responding to HIV among Latinx communities is integral to the success of this initiative. The Latinx community is growing across the United States and not just in coastal or border communities. From 2010 to 2018, more counties in the country’s interior had noticeable increases in their Latinx populations (see maps). More importantly, a significant proportion (31%) of the population in EHE jurisdictions is Latinx, well above the national average of 18%. In some jurisdictions it’s much higher, such as in Miami-Dade County at 69%.
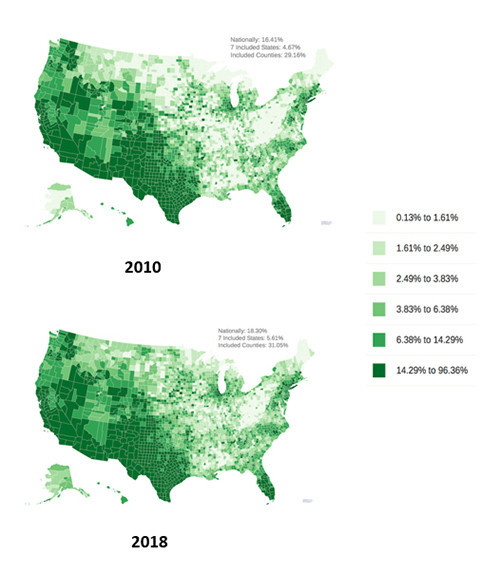
Percent of the U.S. population who are Latinx by county in 2010 and 2018.U.S. Census American Community Survey 5-Year Data / amfAR
In settings such as these, meeting the HIV-related needs of Latinx populations is essential for the EHE plan to have any chance of success. This will include not only expanding access to treatment and to available biomedical HIV prevention options such as the daily pill called PrEP (pre-exposure prophylaxis), but also responding to the contextual and political barriers that Latinx people face when attempting to access care.
While the EHE initiative should be applauded for including jurisdictions with large Latinx populations, the Trump administration has simultaneously supported policies that drive Latinx populations to the margins, making it harder to access healthcare and services and undermining the plan’s chances of success. Over the past three years it has scapegoated undocumented Latinx immigrants and implemented policies targeting both Latinx and LGBT communities.
In doing so, the Administration actively deters people from seeking health services or any form of public assistance for fear of hindering citizenship applications or arrest and deportation. This is especially problematic for people living with chronic conditions like HIV who require consistent access to medical care to support medication adherence and viral suppression. Lack of access to treatment not only subjects people living with HIV to major health complications and even death, but also greatly increases their risk of transmitting the virus to others.
This National Latinx AIDS Awareness day serves as a reminder that we must fight for polices that protect, not marginalize, the communities that most need access to HIV services. This means increasing access to health insurance for Latinx populations for whom rates of uninsurance are among the highest in the nation. Lack of health insurance stymies access to treatment and care, a situation that is further compounded by the fact that five of seven states under the EHE plan have not expanded Medicaid. States that have expanded Medicaid have been shown to make much greater progress in reducing HIV diagnoses.
Nearly four decades into the HIV epidemic, we’ve learned some fundamental lessons. First and foremost, providing access to antiretroviral therapy and keeping people on treatment saves lives and reduces HIV transmission. Similarly, localities that scale up treatment and expand access to prevention options such as PrEP are successful in reducing HIV diagnoses. But despite these successes, HIV disparities remain among marginalized communities, and policies that further marginalize these communities threaten our efforts to meaningfully address HIV.
Perhaps the biggest lesson we have learned is that HIV does not respect borders, nationality, race, sex or any other artificial divisions that people impose on one another. Let’s hope the Trump administration heeds this lesson in time to salvage its signature health initiative.
Zulema Iboa is the Allen Rosenfield HIV/AIDS public policy fellow at amfAR, The Foundation for AIDS Research. This article was originally published at amfAR.org. Go to ehe.amfAR.org to visit the Ending the HIV Epidemic Database.







1 Comment
1 Comment