In an era during which newer first-line antiretroviral (ARV) regimens to treat HIV apparently do not compromise bone mineral density, important research gaps about bone health among people living with the virus and those taking pre-exposure prophylaxis (PrEP) persist. That’s the conclusion of a paper published in Current HIV/AIDS Reports that assesses the research landscape regarding bone health and ARV treatment.
Michael T. Yin, PhD, of Rutgers School of Public Health, led the team that authored the paper.
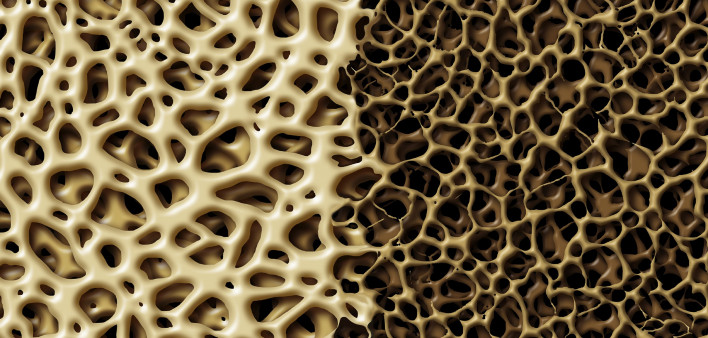
HIV, as well as the immune activation and chronic inflammation caused by the virus, can compromise bone mineral density (BMD). Additionally, starting ARV treatment is associated with an initial decline in BMD that tends to plateau; BMD then improves somewhat within two to three years. This finding came from the randomized controlled global START study, in which most participants who started ARVs received nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), in particular tenofovir disoproxil fumarate, or TDF.
For many years, TDF was the most commonly prescribed ARV in the world, having become the backbone of numerous combination regimens due to its high potency and relatively low toxicity. However, the drug was associated with bone loss. Consequently, Gilead Sciences, which manufactures the drug, released an updated version of the drug, tenofovir alafenamide, or TAF, which in clinical trials has been associated with improved bone mineral density compared with TDF.
That said, other studies have suggested that the actual clinical benefit of TAF over TDF, meaning its ability to prevent fractures, is achieved only when both drugs are used with a boosting agent, either cobicistat or ritonavir.
The new essay’s authors expressed concerns for youth exposed to TDF, either as HIV treatment or in the form of Truvada (TDF/emtricitabine) as PrEP. BMD increases throughout puberty, typically peaks by age 25 and then declines gradually throughout life. Therefore, at least in theory, exposure to TDF during the crucial period of bone development may lead young people to achieve a lower peak level of BMD, leaving them at greater risk for fracture perhaps decades later.
Research indicates that when young people stop taking Truvada as PrEP, their BMD rebounds, although not necessarily completely.
TAF is included in Descovy (tenofovir alafenamide/emtricitabine), which was recently approved in the United States as a new PrEP option. Both Truvada and Descovy were initially approved for use in combination with at least one other ARV to treat HIV. The question of whether Descovy offers a true safety benefit over Truvada when each is used as PrEP is currently the source of considerable controversy.
The authors of the new paper also expressed concerns about how exposure to TDF might affect people as they age and their risk of osteoporosis rises regardless of their HIV status or exposure to ARVs. At this point, switching to a regimen containing either TAF or the bone-friendly abacavir (sold in individual pill form as Ziagen) might not be enough to protect them against advanced bone loss and resulting fractures.
“Significant advances in our understanding of the effect of HIV and antiretrovirals on bone mass and fracture risk during the life span has improved our ability to individualize treatment for [people living with HIV, or PLWH] to mitigate aging-related complications such as osteoporosis and fracture,” the paper’s authors concluded. “Data now support the avoidance of TDF and use of bone-friendly regimens such as [Biktarvy (bictegravir/TAF/emtricitabine)] or [Triumeq (dolutegravir/abacavir/lamivudine)] in PLWH with fracture risks.”
“However,” they continued, “TDF will continue to be utilized as part of combination regimens for HIV therapy and for PrEP and hepatitis B virus (HBV) therapy globally. Certain vulnerable populations, such as children and young adults with HIV from perinatal or behavioral acquisition and older PLWH, are likely to remain at higher risk of fracture despite optimization of [ARV treatment]. Therefore, additional research to define nutritional and lifestyle modifications as well as better biomarkers for risk stratification for fracture risk in this population are needed.”
To read the paper’s abstract, click here.






Comments
Comments