This title may surprise some. In a paper (abstract, below) from a group at CDC I learned yet another HIV/AIDS related acronym. It’s CBWT, Child-to-Breastfeeding-Woman Transmission.
There have been several reports over many years of HIV infected infants born to mothers who were HIV uninfected. These infections were noted as early as the late 1980s in the former Soviet Union, in Libya in 1998, in Kyrgyzstan, Kazakhstan, Romania as well as in Africa. In every instance except in Africa, there cases were investigated with varying degrees of thoroughness. The sources of infection were invariably associated with contaminated blood, either from transfusions, or from procedures in unsafe healthcare settings, where for example sterilization of instruments is inadequate, or injection equipment is reused.
The infections noted in infants that were investigated occurred as outbreaks and all were determined to be nosocomial. Although infected infants born to uninfected mothers have been noted in Africa, remarkably, it appears that none have been investigated.
It will probably remain for a future historian to understand why cases of HIV infection in infants, horizontally rather than vertically transmitted, have yet to be investigated in Africa.
In those non-African outbreaks that were investigated transmission occurred through unsafe medical care, so what do we know of the safety of health care facilities in Africa?
Unfortunately unsafe health care remains a problem in many facilities in high prevalence areas in Africa.
Taking Kenya as an example, Simon Collery has written in one of my blogs:
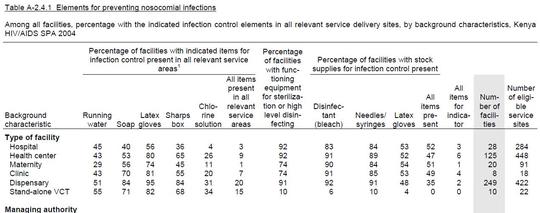
Where does Kenya fit into this picture? As UNAIDS admit, there’s not much data. But there is a document called the Service Provision Assessment which looks at conditions in various kinds of health facility, such as hospitals, clinics and pharmacies.
A few samples from this document may suffice to illustrate Kenya’s capacity to prevent HIV transmission through unsafe injections and other healthcare practices: Between 10 and 15% of facilities don’t have adequate supplies of needles, syringes or latex gloves; between 55 and 70% don’t have running water or soap; many don’t have facilities for disposing of contaminated equipment or supplies of disinfectant; less than half have guidelines for infection prevention and less than 10% have guidelines for sterilization.
Although this document dates from 2004, we don’t know if there has been any change.
As the title of this post indicates, infants infected either vertically or through exposure to contaminated blood are able to transmit HIV to seronegative women who breast feed them.
Mother to child transmission is the leading cause of HIV infection in infants. Some of these infected infants will be orphans and so place seronegative women who breastfeed them at risk. Wet-nursing is the complete nursing of another woman’s infant and still occurs as does cross-nursing which is the nursing of another infant by a woman while still nursing her own child. Estimates of the prevalence of these practices vary by region and the overall prevalence is not known.
Worldwide the greatest risk for CBWT is carried by seronegative mothers whose infants become infected through exposure to contaminated blood. Rates of CBWT were as high as 40-60% among mothers breastfeeding infants who became infected after birth. (noted in the paper referenced below).
This report on CBWT highlights the importance of unsafe health care facilities in the transmission of HIV. Of course HIV is not the only pathogen that can be transmitted in such settings.
Why so few resources have been devoted to the improvement of health care facilities in developing nations is puzzling. Could it be that like the provision of clean water and sanitation, improving health care facilities is not something that can generate much profit?
Perhaps it will be left to HIV activists who have successfully drawn public attention to other neglected issues, to alert funders and policy makers to the dangerous condition of many healthcare facilities in the developing world.
The benefits of improving infection control in these facilities extend far beyond effects in HIV transmission.
A group of individuals have been trying to bring attention to this issue for many years and I do recommend looking at the website they have created to directly alert people in Africa to dangers in health care facilities with no or poor infection control procedures.
I realize I neglected one point, exposure to saliva is not considered to be a great risk for HIV transmission, so why is it happening in the case of CBWT?
The authors suggest maternal skin fissures or infant stomatitis (inflammation of the lining of the mouth). I’m not aware of research that would explain such transmissions in infancy. I hope it will be undertaken.
(1) A Review of Evidence for Transmission of Human Immunodeficiency Virus from Children to Breastfeeding Women and Implications for Prevention.
Kirsten M Little, Peter Kilmarx, Allan Taylor, Charles Rose, Emilia Rivadeneira. And Steven Nesheim.
The Pediatric Infectious Disease Journal Publish ahead of print.
DOI:10.1097/INF.0b013e318261130f
Abstract
Background: Child-to-Breastfeeding-Woman Transmission (CBWT) of HIV occurs when an HIV-infected infant transmits the virus to an HIV-uninfected woman through breastfeeding. Transmission likely occurs as a result of breastfeeding contact during a period of epithelial disruption, such as maternal skin fissures and/or infant stomatitis. Despite extensive epidemiologic and phylogenetic evidence, however, CBWT of HIV continues to be overlooked.
Objective: This paper summarizes the available evidence for CBWT from nosocomial outbreaks, during which nosocomially HIV-infected infants transmitted the virus to their mothers through breastfeeding. This paper also explores the CBWT risk associated with HIV-infected orphans and their female caretakers, and the lack of guidance regarding CBWT prevention in infant feeding recommendations.
Methods: We searched online databases including PubMed and ScienceDirect for English language articles published from January 1975 to January 2011 using the search terms “HIV”, “perinatal”, “child-to-mother”, and “breastfeeding”. The citations from all selected articles were reviewed for additional studies.
Results: We identified five studies documenting cases of CBWT. Two studies contained data on the number of HIV-infected women, as well as the proportion breastfeeding. Rates of CBWT ranged from 40 - 60% among women reporting breastfeeding after their infants were infected.
Conclusions: Poor infection control practices, especially in areas of high HIV prevalence, have resulted in pediatric HIV infections and put breastfeeding women at risk for CBWT. Current infant feeding guidelines and HIV prevention messages do not address CBWT, and fail to provide strategies to help women reduce their risk of acquiring HIV during breastfeeding.







12 Comments
12 Comments