Having a low mood is common—especially in these challenging times—but people with HIV often experience more persistent feelings of sadness or depression, even under normal circumstances.
Many aspects of living with HIV can contribute to depression, including fear of illness and death, loss of loved ones, survivor’s guilt, decreased self-esteem related to body changes, chronic pain, difficulty performing daily activities and struggles with stigma.
Depression can range in severity from mild feelings of sadness to a persistent, severe depressed mood. Clinical depression, also known as major depressive disorder, is distinct from temporary sadness related to an event such as the death of a family member. It can last longer and interfere with daily life.
According to the National Institute of Mental Health, people with chronic illnesses, such as HIV, heart disease or cancer, are more likely to experience depression compared with the general population, and depression can lead to worse disease outcomes.
Depression is a real medical condition that can have serious consequences. Feelings of depression, low self-worth or hopelessness can contribute to poor adherence to antiretroviral treatment, resulting in HIV disease progression.
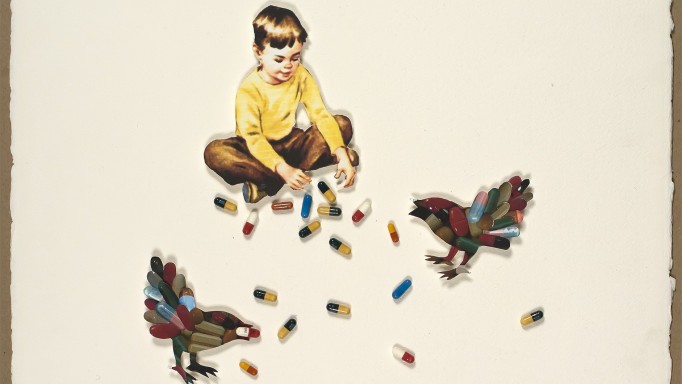
In some cases, depression may lead people to seek relief through excessive use of alcohol, recreational or street drugs or risky sexual activity.
If you are experiencing persistent depression, it may be time to seek help. If you have thoughts about self-harm or suicide, get help right away.
Start by talking with your primary health care provider about getting a psychological evaluation and treatment, if appropriate. You may be referred to a psychologist, psychiatrist or other mental health specialist.
Doctors use a list of symptoms from the Diagnostic and Statistical Manual of Mental Disorders to determine whether someone has clinical depression. These include:
- A depressed or sad mood
- Loss of interest and pleasure in most activities
- Changes in appetite or unintentional weight loss or gain
- Insomnia or excessive sleepiness
- Poor concentration or impaired ability to think
- Fatigue, unusual tiredness or low energy
- Moving, talking or thinking more slowly
- Feeling restless and unable to sit still
- A sense of worthlessness or guilt
- Recurrent thoughts about death or suicide.
Diagnosis and Treatment
Diagnosing depression involves ruling out physical problems that can affect mood—for example, a low testosterone level or an underactive thyroid gland. In people with advanced immune suppression, opportunistic infections that attack the brain can contribute to changes in mood and behavior. Medication side effects may also play a role. The antiretroviral efavirenz (Sustiva, also included in the Atripla combination pill) has been linked to depression and other neuropsychiatric symptoms.
Sometimes talking with a psychologist or other trained therapist may be enough to lift your mood. Evidence-based psychotherapy approaches for depression include cognitive behavioral therapy and interpersonal therapy. Many people also find group therapy or peer support groups helpful.
In some cases, antidepressant medications may be needed. A variety of drugs that work in different ways—often acting on neurotransmitters that enable neurons in the brain to communicate—are used to manage depression. Antidepressants can cause side effects, including drowsiness, constipation and changes in sexual function. Some can interact with certain HIV medications, so it’s important for your providers to work together to find a safe regimen.
Antidepressants can take time to start working (usually two to six weeks), and they are not equally effective for everyone. However, many people who do not respond to one medication will do well on another. It often takes considerable trial and error to find the right regimen, but in a majority of cases, depression can be successfully treated.
In addition to psychotherapy and antidepressants, there are other steps you can take to lessen feelings of depression, including exercise, eating a healthy diet, getting enough sleep and spending time with others. Studies show that HIV-positive people who have little social support are more likely to experience depression, and depression in turn can lead to social isolation.
Maintaining social connections and avoiding isolation can be especially challenging now, given the physical distancing and limits on social activities required to slow the spread of COVID-19. Alternative ways of connecting with others include social media, online chat forums and simply picking up the phone to talk to a family member or friend.
Last Reviewed: November 12, 2020