The U.S. Centers for Disease Control and Prevention (CDC) has reported troubling signs that gonorrhea may develop resistance to the only recommended treatment of the sexually transmitted infection (STI). The rate of what is known as reduced susceptibility to the key antibiotic azithromycin increased four-fold between 2013 and 2014—a warning of the potential for actual drug resistance that could result in treatment failures and potentially the spread of untreatable gonorrhea.
Publishing their findings in the Morbidity and Mortality Weekly Report, researchers analyzed data from the Gonococcal Isolate Surveillance Project (GISP), studying 5,093 isolates of gonorrhea collected in 2014 from men with gonococcal urethritis visiting STI clinics at 27 sites across the United States.
An estimated 800,000 new infections of gonorrhea occur annually in the United States, and fewer than half of them are diagnosed. In 2015, the CDC reported that gonorrhea and other STIs, including syphilis and chlamydia, are on the rise, especially among men who have sex with men (MSM).
Left untreated, gonorrhea can lead to serious health problems, especially for women who may experience chronic pelvic pain, life-threatening ectopic pregnancy and infertility. The STI also raises the risk of both transmitting and acquiring HIV.
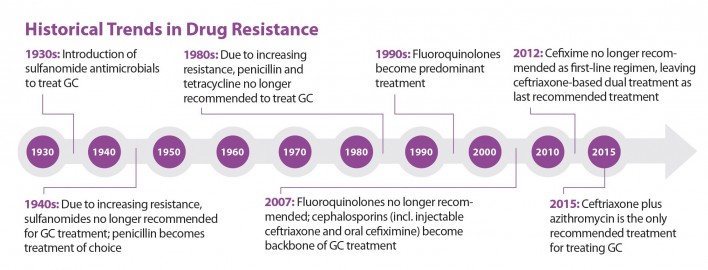
Currently, the only recommended gonorrhea treatment is dual therapy with the antibiotics ceftriaxone and azithromycin. This combination is still effective; thus far, there have been no reports of anyone failing the treatment. However, throughout history, gonorrhea has developed resistance to a long line of other antibiotics used to treat the STI, including penicillin, tetracycline and the fluoroquinolone class.
During the 2010s, the CDC has twice switched the recommended treatment for gonorrhea. In 2010, responding to increasing resistance to cefixime, the CDC began recommending a drug from the cephalosporin class, which includes cefixime, plus a second antibiotic. Drug resistance to cefixime subsequently decreased. In 2012, the CDC stopped recommending cefixime as part of first-line treatment, resulting in the current first-line treatment recommendation.
Of the isolates collected in 2014 for the new CDC study, 25.3 percent were resistant to tetracycline, 19.2 percent to ciprofloxacin and 16.2 percent to penicillin. The percentage of isolates that were resistant to tetracycline, ciprofloxacin, penicillin or to all three were greater in those taken from MSM than men who have sex with women.
Between 2013 and 2014, reduced susceptibility to azithromycin, one of the two drugs in the current recommended first-line treatment for gonorrhea, increased from 0.6 percent to 2.5 percent of isolates. This four-fold increase is “a distressing sign that the future of current treatment options may be in jeopardy,” according to the CDC. Rates rose in all geographic regions of the country, but the increases were the greatest in the Midwest. Men who have sex with women, with men, and with men and women all experienced this increase. Among the isolates that had reduced susceptibility to azithromycin, none had reduced susceptibility to cefixime or ceftriaxone.
The study authors state that it is unclear whether the recent increase in the rate of gonorrhea with reduced susceptibility to azithromycin is the beginning of a trend. Nevertheless, Jonathan Mermin, MD, director of the CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD and Tuberculosis Prevention, stressed in a press release: “The confluence of emerging drug resistance and very limited alternative options for treatment creates a perfect storm for future gonorrhea treatment failure in the United States. History shows us that bacteria will find a way to outlast the antibiotics we’re using to treat it. We are running just one step ahead in order to preserve the remaining treatment option for as long as possible.”
If strains of gonorrhea do become resistant to azithromycin, the ceftriaxone component of treatment may still cure the infection. But the threat always remains that azithromycin-resistant strains of gonorrhea may become resistant to ceftriaxone as well.
“It is unclear how long the combination therapy of azithromycin and ceftriaxone will be effective if the increases in resistance persist,” said Gail Bolan, MD, director of the CDC’s Division of STD Prevention, in the same press release. “We need to push forward on multiple fronts to ensure we can continue offering successful treatment to those who need it.”
There are several drug trials of new, investigative treatments of gonorrhea currently under way. However, there is no guarantee these drugs will be safe and effective. And even if they are, years may pass before they are approved.
According to previous years of the GISP, reduced susceptibility to cefixime increased from 0.1 percent in 2006 to 1.4 percent in both 2010 and 2011. This rate then dropped to 0.4 percent in 2013 but increased again to 0.8 percent in 2014. The rate of reduced susceptibility to ceftriaxone followed a rather similar pattern, increasing from 0.1 percent in 2008 to 0.4 percent in 2011 and falling to 0.1 percent in 2013 and 2014.
The study authors write that despite the drop in the rate of isolates with reduced susceptibility to cefixime during 2012 and 2013, the subsequent increase in 2014 “underscores the potential threat” of gonorrhea strains becoming resistant to the cephalosporin antibiotic class, including cefixime.
“The growing threat of untreatable gonorrhea, combined with increasing rates of disease, makes it more important than ever to prevent new infection,” Mermin said in the press release. “There is a critical need to strengthen STD prevention services. Gonorrhea and other STDs can currently be prevented, diagnosed and treated—action today is essential to prevent worse outcomes tomorrow.”
Because the CDC study focused on 2014, when the use of Truvada (tenofovir disoproxil fumarate/emtricitabine) as pre-exposure prophylaxis (PrEP) remained uncommon among MSM, it is unlikely PrEP’s introduction affected the rate of susceptibility to azithromycin among the gonorrhea isolates studied. However, the CDC stresses that it is important for MSM, including those on Truvada for prevention, to discuss how to reduce their risk for STIs, including through regular testing.
To read a POZ feature about how condom use affects the risk of STIs, click here.
To read the CDC press release, click here.
To read the MMWR, click here.
Courtesy of CDC







Comments
Comments