An ongoing study of young gay and bisexual men in New York City found that among those who ever took pre-exposure prophylaxis (PrEP), individuals reported more recent condomless sex with casual partners at the points in the study when they were taking Truvada (tenofovir disoproxil fumarate/emtricitabine).
Researchers from the Center for HIV Education Studies & Training (CHEST) at Hunter College in New York City analyzed 2014 to 2016 data from the One Thousand Strong study. The longitudinal study included 1,071 HIV-negative young men age 18 and older who identified as gay or bisexual and lived in the United States.
Findings were presented at the 9th International AIDS Society Conference on HIV Science in Paris (IAS2017).
Once annually, the investigators sent self-testing packages to the participants with an instructional video on how to collect samples from the urethra and rectum to be tested for gonorrhea and chlamydia. The participants also reported whether they had ever been prescribed PrEP and whether they were currently taking it.
A total of 71.2 percent of the participants were white; 95 percent identified as gay; 67.2 percent were fully employed; the income brackets were fairly evenly distributed, with 33.8 percent making $20,000 to $49,000 per year and 27.5 percent making more than $74,000 per year; 55.7 percent had a college degree or higher; and 48.7 percent said they were in a relationship.
Between April and October 2014, 1,033 participants sent samples for STI testing an provided survey responses. The 12-month study time point included 913 participants from that first group; 810 remained at the 24-month point.
PrEP did not start gaining in significant popularity in the United States until 2014.
The participants used PrEP at increasing rates during the study. The rate of those reporting past PrEP use also rose. At the baseline, 12-month and 24-month time points, the respective proportions reporting that they had never been on PrEP were 96.5 percent, 90.1 percent and 82.5 percent. The respective proportions reporting current PrEP use at each time point were 2.9 percent, 8.1 percent and 14.4 percent. And finally, the respective proportions at each time point reporting that they were not currently on PrEP but had taken it before were 0.01 percent, 1.8 percent and 3.2 percent.
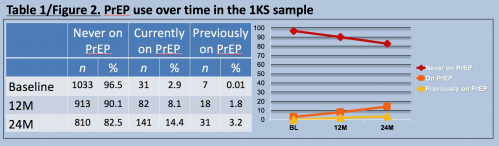
The number (“n”) and percentage of participants at the study’s three time points—baseline (BL), 12-month (12M) and 24-month (24M)—that reported that that they had never taken PrEP, were currently on PrEP or had previously taken PrEP.Jeffrey T. Parsons, PhD, Hunter College, CUNY; CHEST
The study authors used to means to analyze the data on STI diagnoses and the participants’ reported recent condomless anal sex with casual partners. For the first method, they divided everyone into three groups: those reporting at each of the three time points that they had never taken PrEP, were taking PrEP or had taken PrEP in the past. The investigators then compared the groups’ varying rates of STI diagnoses and condomless anal sex at each of the three time points.
There were statistically significant differences between the groups (meaning the differences were unlikely to have been driven by chance) when it came to rates of recent casual condomless sex. The researchers saw this difference at the baseline and 12-month points, with those currently taking PrEP having the highest rates of such sex at both times. There were also statistically significant differences in STI diagnosis rates between the groups at the 12-month and 24-month points, with those who had never taken PrEP by far the least likely to receive such a diagnosis.

Researchers lumped into groups those never on PrEP, currently on PrEP and previously on PrEP at the study’s three time points—baseline (BL), 12-month (12M) and 24-month (24M)—to compare the proportion who at those times reported condomless anal sex (CAS) Jeffrey T. Parsons, PhD, Hunter College, CUNY; CHEST
The researchers also analyzed shifting patterns in STI diagnoses and casual condomless anal sex reporting within each of the three groups. Looking just at those who reported ever using PrEP at one time point or more during the study, they found a significant increase in the rate of casual condomless anal sex during the points when the men reported being on PrEP. Specifically, at the time points when these men reported current PrEP use they reported a 2.52-fold higher rate of casual condomless sex than at the time points when they did not report current PrEP use.
Those who in the group that ever used PrEP who discontinued Truvada during the study reported a 12 percent lower rate of recent casual condomless sex than at the time points when they reported current PrEP use, although this decline was not statistically significant.
PrEP’s apparent effect on increased sexual risk-taking was particularly strong when looking at reported rates of condomless anal sex with HIV-positive partners. Among those who ever took PrEP, at the visits when they reported current Truvada use, they had a 12.38-fold higher rate of reporting such sexual activity than at points when they were not taking the prevention medication.
Still looking just at the ever users of PrEP, the investigators found that compared with time points when they reported no PrEP use, these men were 58 percent more likely to receive an STI diagnosis at the time points when they reported active Truvada use and 22 percent more likely to receive such a diagnosis at points when they reported having discontinued PrEP. However, these differences were not statistically significant.
The researchers believe that their study is limited by the fact that participants who took PrEP were early adopters of Truvada for prevention who may have started the prevention medication with a higher level of recent sexual risk-taking than those starting PrEP at later times. Larger studies of individuals with less risky sexual patterns upon starting PrEP are needed to better examine how Truvada may affect their own behavioral patterns and STI diagnoses.







Comments
Comments