The estimated annual number of new HIV infections in the United States fell 18 percent between 2008 and 2014. Stagnant at about 45,000 to 50,000 per year since the mid-1990s, the Centers for Disease Control and Prevention’s (CDC) estimate of HIV incidence fell from 45,700 to 37,600 during this recent six-year period.
Findings from the CDC’s new analysis, including a report that focused specifically on HIV rates among men who have sex with men (MSM), were presented at the 2017 Conference on Retroviruses and Opportunistic Infections (CROI) in Seattle. The CDC arrived at its estimates by analyzing HIV diagnosis data as well as post–HIV diagnosis CD4 counts reported to the National HIV Surveillance System between 2008 and 2014. Researchers used mathematical models to estimate how long individuals had been infected by the time they were diagnosed based on their CD4 count.
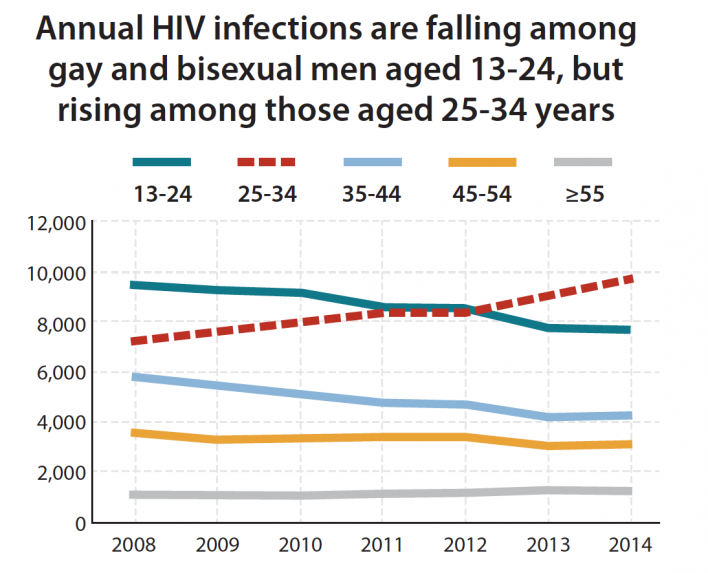
CDC researchers estimated that between 2008 and 2014, HIV infection rates declined: 56 percent among injection drug users, from 3,900 to 1,700; 36 percent among heterosexuals, from 13,400 to 8,600; 18 percent among young MSM ages 13 to 24, from 9,400 to 7,700; and 18 percent among white MSM, from 9,000 to 7,400. MSM as a whole were the only major risk category that did not see a decline during the six-year period; the HIV incidence for this group remained stable, a finding that was still promising news, since during the preceeding years the HIV rate rose among MSM.
Courtesy of CDC
Looking specifically at certain states, the CDC estimated that over the six-year period HIV rates fell 10 percent annually in Washington, DC, 8 percent annually in Maryland, 7 percent annually in Pennsylvania, 6 percent annually in Georgia, 5 percent annually in both New York and North Carolina, 4 percent annually in Illinois and 2 percent annually in Texas. Among all 35 states (including Washington, DC) analyzed, the CDC found none that saw increasing HIV rates during the study period; all saw falling or stable HIV incidence.
The CDC attributes much of the HIV incidence decline to successful efforts to increase the proportion of those living with the virus who are diagnosed, on treatment and virally suppressed. A large body of research has shown that an undetectable viral load is associated with an extremely low risk of transmission of the virus; the risk may in fact be zero.
In addition, CDC officials believe that the advent of PrEP—which was approved in 2012 and after a slow start began to gain in popularity in 2013, largely among white MSM older than 25—may have contributed to dropping HIV rates in more recent years.
The new analysis also found regional disparities in estimated HIV incidence. Although the South is home to only 37 percent of the U.S. population, 50 percent of estimated new HIV infections in 2014 were in Southern states.
In a press release, Jonathan Mermin, MD, director of the CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, addressed concerns about the expanding opiate addiction in the United States.
“The opioid epidemic in our country is jeopardizing the dramatic progress we’ve made in reducing HIV among people who inject drugs,” Mermin said. “We need to expand the reach of comprehensive syringe services programs, which reduce the risk of HIV infection without increasing drug use and can link people to vital services to help them stop using drugs.”

Courtesy of CDC
For the CDC press release, click here.
For a fact sheet about the overall HIV incidence analysis, click here.
For a fact sheet on state-by-state HIV incidence rates, click here.
For a POZ feature article on how the Trump administration may affect the future of syringe services programs for IDUs, click here.







Comments
Comments