We have made tremendous progress in terms of reducing the risk of mother-to-child transmission. Provided that a woman living with HIV takes good care of herself and her developing baby, which includes getting proper prenatal care and taking a combination of HIV medications during pregnancy, labor and delivery—the risk of HIV transmission is less than 2 percent.
Today, thanks to early access to care and advances in HIV drug treatment, being a child living with HIV is not nearly as dire as it once was. And with more information quickly emerging with respect to how children living with HIV should be treated, we can expect the success rate to improve significantly.
Nonetheless, caring for a child who is HIV positive comes with many challenges. HIV, even during the earliest stages of infection, can severely affect a child’s development, whether related to physical growth, psychological evolvement, or emotional well-being.
Children have different immune systems than adults. HIV rapidly impairs a child’s immune system ability to control common childhood infections, such as bacterial-associated lung and ear infections and viral infections like chicken pox. HIV also prevents the immune system from producing memory cells which, in adults, help ward off life-threatening infections like Pneumocystis pneumonia (PCP), Mycobacterium avium complex (MAC), and cytomegalovirus (CMV). What’s more, many children living with HIV are born to mothers who abused alcohol and/or drugs while pregnant, which can worsen problems caused by HIV infection.
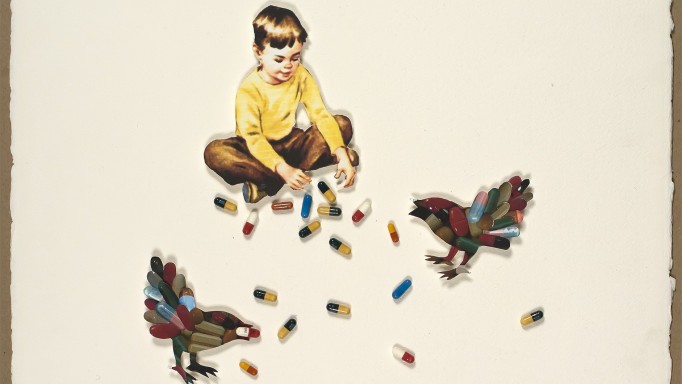
Researchers have shown that babies with HIV tend to have higher viral loads than adults. As a result, the lessons we have learned about treating adults with HIV hold true for children infected with the virus: a powerful combination of drugs should be used to lower a child’s viral load to the lowest possible level.
Are HIV meds safe for children?
Many clinical trials have determined that some HIV drugs, particularly when used in combination with each other, work well and are safe in children. However, it is important to recognize that many HIV drugs are absorbed, metabolized and eliminated from the body differently in children than in adults. Fortunately, many of the drugs used to treat adults with HIV can also be used to treat children with HIV infection. In fact, many have also been found to be safe and effective for newborns and infants infected with the virus.
When should children start HIV treatment?
The United States Department of Health and Human Services (DHHS)—a branch of the federal government that oversees health care policy in the United States—has published guidelines focusing on how best to treat HIV-positive children. These guidelines are important, as they help to make sure that all HIV-positive children in the United States are sufficiently cared for and treated.
The guidelines, which were updated in April 2019, are based on data collected from a number of studies—along with expert opinions—focusing on the importance of treating HIV-positive children, including the best time to start treatment and the best treatments to use.
Click here for the DHHS recommendations of when HIV treatment should be started by HIV-positive children.
If you are caring for a child living with HIV who is not being treated or have questions about starting your child on antiretroviral medications, be sure to discuss these issues with your child’s pediatrician.
Once HIV treatment is started, the child living with HIV will need to be monitored regularly to make sure that the medications are working well and not causing any serious side effects. If a significant problem arises while on therapy—such as a viral load becoming and/or remaining detectable, suppression of the immune system, symptoms of infection, slowed development of the central nervous system or growth failure —a switch in therapy might be necessary.
What drug combinations are recommended for children?
As is the case with adults infected with HIV, children living with HIV almost always need to be treated with a combination of drugs to help push their viral loads to undetectable levels. This helps delay drug resistance, prolong the effects of treatment and keeps the immune system functioning properly.
Click here for the DHHS treatment guidelines on what regimens are recommended for initial therapy of children living with HIV.
What about opportunistic infections?
As with adults, children living with HIV need to take preventive therapies (prophylaxis) to ward of common childhood and AIDS-related infections. It’s estimated that 20 percent of children living with HIV will have an opportunistic infection within the first year of their life.
All children less than 1 year of age must take Bactrim or Septra (TMP-SMX)—or if they are allergic to sulfa-based drugs, either dapsone or aerosolized pentamidine (NebuPent)—to prevent Pneumocystis pneumonia (PCP). Children between the ages of 1 and 2 should take PCP prophylaxis if their CD4 cells fall below 750. Two- to five-year-olds with CD4 cell counts below 500 should also be taking prophylaxis, as should all children six years or older with CD4 counts below 200 (similar to adult recommendations).
A rather unique HIV-related problem among children is lymphoid interstitial pneumonitis (LIP). LIP is caused by a hyperactive immune response to a usually harmless infection in the lungs. The symptoms are similar to those of asthma (e.g., coughing, wheezing, shortness of breath, tightness in the chest) and, likewise, are treated with corticosteroids like prednisone, and with inhalers to ease breathing.
Conclusion
While research continues to show that HIV therapy has made a tremendous impact on the lives of children living with HIV, it’s not yet entirely understood to what extent these powerful drugs affect young immune systems. In turn, maintaining children on treatment remains the standard of care, and it is still not clear whether or not immune system-related complications, such as LIP, are less likely to occur during successful HIV therapy.
The bottom line is that the care and treatment of our youngest patients with HIV has come a long, long way in recent years. While it will take some time to sort out the unique complications facing children living with HIV, fortunately, time is one thing many of those children now have.
Last Reviewed: April 16, 2019