Toxoplasmosis is a disease caused by the parasite Toxoplasma gondii, which can be found throughout the environment. Infection with toxoplasmosis does not mean that a person will develop active disease; but when it does, toxoplasmosis usually affects the brain causing a disease called toxoplasmic encephalitis. The parasite can infect and cause disease in other organs, including the eyes and lungs.
Nearly 40 million living in the United States have been exposed to the parasite at some point in their lives. However, people with weakened immune systems—including people with HIV with CD4 counts below 50—are at risk for developing toxoplasmosis disease. Women who become infected just before or during pregnancy can pass toxoplasmosis onto the unborn child.
Common sources of this organism include cats or birds, undercooked meat (especially beef, pork, lamb, or venison), and raw shellfish. While cats or birds that test negative for toxoplasmosis and remain housebound are not a risk, those that go outside can carry it back into the house or apartment. Coming into contact with bird or cat droppings is a major source of infection.
Encephalitis can occur in people who have antibodies to toxoplasmosis, which shows that the infection is present in the body. The disease is rare among people with HIV with CD4 counts above 200, and is most common when CD4 counts fall below 50. Luckily, some of the treatments used to prevent Pneumocystis pneumonia (PCP) can also prevent T. gondii from causing disease.
What are the symptoms, and how is it diagnosed?
Initial infection with toxoplasmosis usually doesn’t show symptoms. If present, they’re usually mild flu-like symptoms. Symptoms of toxoplasmic encephalitis include headache, fever, confusion, muscle weakness, seizures, abnormal behavior, and coma.
A blood test can be done to check for antibodies to T. gondii (including on cats and birds). Most cases of disease occurs from a reactivation of an earlier, latent infection. In some cases, active disease can be caused by a recent exposure, perhaps from eating undercooked meat.
To diagnose toxoplasmic encephalitis, three parts are needed: 1) a positive antibody result, 2) T. gondii lesions found on a CT or MRI scan, and 3) current symptoms consistent with toxoplasmosis. It can be difficult to tell the difference between toxoplasmosis and other central nervous system disease, such as lymphoma, so newer imaging devices (such as PET or SPECT scans) can help correctly diagnose the condition.
If toxoplasmosis of the brain is suspected, treatment will likely be started immediately, even if doctors can’t confirm the diagnosis. A brain biopsy will be done to establish the diagnosis only if the person does not respond to treatment. A biopsy may be required to diagnose toxoplasmosis in other body tissues, such as the lungs.
How is it treated?
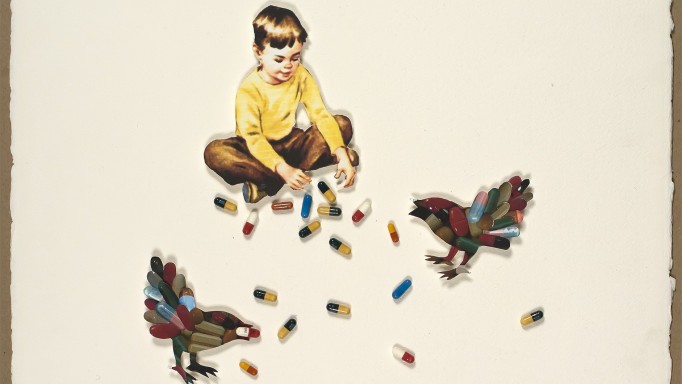
To treat toxo, three drugs are usually recommended, amounting to more than ten pills a day:
- Pyrimethamine (Daraprim): A large dose (100 mg to 200 mg) of this antimalarial drug is taken at first, followed by a lower dose. It is taken by mouth in pill form.
- Leucovorin: This medication contains folate, the active form of the B complex vitamin. Because pyrimethamine can decrease folic acid levels in the body, which can reduce the formation of red and white blood cells, leucovorin is used to protect against anemia and other toxicities.
- Sulfadiazine: This antibiotic is taken by mouth four times a day.
High doses of these treatments are continued for 4–6 weeks. Thereafter, lower doses are taken as “maintenance therapy” to prevent the toxoplasmosis from coming back. Maintenance therapy can be stopped if you have completed the first six weeks of treatment and no longer have symptoms of toxoplasmosis —provided that your CD4 cell count is above 200 for at least three months while taking HIV meds.
An alternate regimen is pyrimethamine + clindamycin + leucovorin, used for those who are allergic to sulfadiazine. Atovaquone may also be used.
Corticosteroids are sometimes used to help control inflammation of the brain and the symptoms associated with toxoplasmosis. However, these need to be used carefully and stopped when possible. Anticonvulsants may also be used for people with a history of seizures while treating toxoplasmosis.
Can it be prevented?
Yes. For people who do not have antibodies to T. gondii or do have antibodies but no longer have the infection (determined using PCR), the best way to prevent toxoplasmosis is not to come into contact with the parasite. Wash hands after touching raw meats or shellfish or handling soil. Wash raw fruits and vegetables well before eating.
Meats, such as pork, beef, lamb, or venison, should never be eaten rare and should be cooked long enough so that the internal temperature is 150°F. This is especially true for people with HIV with CD4 counts below 100.
As for cats and birds, it’s best to use rubber gloves when cleaning litter boxes or removing droppings from cages. This is especially true for pregnant women, to prevent infection to herself and to the unborn baby. It’s best to clean up after these pets every day because T. gondii is not infectious in fresh cat or bird excrement—it takes a couple days for the parasite’s eggs to hatch while inside cat or bird feces. Cats and birds can be tested for T. gondii antibodies, and then always keeping them inside can also reduce the risk of exposure.
Drugs used to prevent toxoplasmosis are, for the most part, the same as those used to prevent PCP. Trimethoprim-Sulfamethoxazole (TMP-SMX; Bactrim, Septra, Cotrim) is the most effective medication used. And because PCP preventive treatment is generally started when a person’s CD4 count falls below 200, he or she is well protected against toxoplasmosis should the CD4 count fall below 100.
For those who cannot handle TMP-SMX, due to the allergic reactions caused by SMX, another effective option is dapsone with pyrimethamine and leucovorin. This triple-drug combination is taken once a week. Atovaquone may also be used.
People who have been taking preventive treatment for toxoplasmosis and whose CD4 count stays above 200 for at least six months can stop preventive treatment. However, for people whose CD4 count never rises above 200, lifelong use of preventive treatment is likely necessary.
Are there any experimental treatments?
If you would like to find out if you are eligible for any clinical trials involving new treatments for toxoplasmosis, visit ClinicalTrials.gov, a site run by the U.S. National Institutes of Health. The site has information about all HIV-related clinical studies in the United States. For more info, you can call their toll-free number at 1-800-HIV-0440 (1-800-448-0440) or email contactus@aidsinfo.nih.gov.
Last Reviewed: October 23, 2018