These have been exciting times for HIV prevention, with pre-exposure prophylaxis (PrEP) making an impact and science finally proving that successfully treating the virus blocks transmission. And now, promising new vaccine candidates have made their way into a trio of major late-stage efficacy trials.
Two of these trials have launched in sub-Saharan Africa in recent years. One, called Imbokodo, started enrolling at-risk women in 2017, was fully enrolled by May 2019 and will likely report its first findings in late 2021.
Now at-risk transgender people and cisgender men who have sex with men (MSM) in the Americas and Europe will have a chance to participate in a new vaccine study called Mosaico.
Those who join the study may wind up being the first to receive what proves to be an at least moderately effective vaccine. Regardless of the trial’s outcome, their participation will surely contribute invaluable knowledge to the global HIV prevention research effort.
This fall, the Mosaico HIV vaccine trial will start enrolling a planned 3,800 18 to 60-year-old cisgender men and transgender or gender-nonconforming individuals who have sex with men, with trans people or both and who are at significant risk of contracting the virus. The trial will operate out of more than 55 clinical research sites in the United States, Mexico, South America and Europe.

Mosaico study site locations
Also called HVTN 706 or HPX3002, Mosaico is a multicenter, randomized, double-blind, placebo-controlled Phase III efficacy study that will test a four-part vaccine—with injections spread out over 12 months—similar to the regimen under investigation in Imbokodo.
Mosaico is projected to complete during the first half of 2023.
The trial is the product of a public-private partnership between Janssen and the HIV Vaccine Trials Network (HVTN), headquartered at the Fred Hutchinson Cancer Research Center in Seattle. The National Institute of Allergy and Infectious Diseases (NIAID) is providing funding and other forms of support as well as guidance.
Thanks to PrEP’s high efficacy, designing an HIV prevention trial has become a complex challenge in recent years. On the one hand, it is not ethical for such trials to deny participants an existing prevention method that is so powerful. But on the other hand, prevention trials must enroll people who remain at significant risk of contracting the virus over an extended period, otherwise they won’t be able to prove that the experimental prevention agent reduces such risk when compared with a placebo.

PrEPIstock
After careful consultation with numerous community stakeholders, the Mosaico design team decided that to be eligible to participate in the trial, applicants must not be taking Truvada (tenofovir disoproxil fumarate/emtricitabine) for prevention at the time they enter the screening process. They also may not have received long-acting injectable PrEP, a still-investigational HIV prevention modality, during the two years prior to the administration of the first vaccine injection.
That said, during the Mosaico screening process, potential participants will be offered access to PrEP. The Mosaico architects are ensuring that there will be systems in place, including the availability of PrEP navigators, so that all will be able to access the prevention pill—in some cases through local studies, called demonstration projects, of real-world PrEP use.
“We want the original decision to be an authentic choice,” Susan Buchbinder, MD, the Mosaico protocol chair and director of Bridge HIV at the San Francisco Department of Health, says of applicants’ motivation for entering the trial. “We didn’t want people to say, ‘Oh, well, I can’t get PrEP, so I want to be in the trial.’”

Susan P. Buchbinder of UCSF at the 2017 Conference on Retroviruses and Opportunistic Infections in SeattleCourtesy of Benjamin Ryan
Those who opt not to take PrEP during screening and are otherwise deemed eligible may enter the vaccine trial. However, at any time after receiving the first vaccination shot, they are free to choose to go on PrEP. Post-exposure prophylaxis (PEP) will also be an option for participants.
Additionally, participants will receive ongoing HIV risk reduction counseling, condoms and lube, and sexually transmitted infection testing and treatment.
At least in theory, a vast majority of participants could go on PrEP during the study and adhere well to that regimen—making it impossible to determine the true efficacy of the vaccine.
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases (NIAID), says that knowledge of human nature suggests that such a scenario is highly unlikely.
Indeed, the study is designed to select for people who are at significant risk of contracting HIV and who prefer not to take PrEP even when offered easy access—in other words, individuals who most need a new prevention method that works with their preferences and who are most likely to benefit from an effective vaccine. Consequently, Mosaico is considered to have clinical equipoise, or an ethical balance in its trial design.
After a 45-day screening period, participants will be randomized to receive the vaccine or a placebo, given in four injections spread out over 12 months—specifically on day 1 and then at months 3, 6 and 12.

Istock
Known as Ad26.Mos4.HIV, the vaccine uses an engineered adenovirus vector—a harmless relative of the common cold virus—to deliver HIV proteins (antigens) designed to prompt an immune response. The third and fourth injections include a booster against a wide variety of HIV strains.
All participants who remain HIV negative will be followed until the last study member reaches at least the 24-month mark (various factors may lead the investigators to extend this to the 30-month mark). Those who test positive for the virus will be followed for six months following their diagnosis.
This summer, the HIV research community learned of the promising findings from the mid-stage human studies APPROACH and ASCENT, which between them, along with another study, TRAVERSE, investigated vaccine regimens that were ultimately advanced to Mosaico and Imbokodo. All the studies showed that the preferred regimens prompted strong, durable immune responses among participants.
What’s more, the level of HIV antibodies seen in participants who received these vaccines exceeded the threshold found to be protective against the simian version of the virus in the nonhuman primate research.

Istock
These findings have inspired, at a minimum, cautious optimism among the designers of Imbokodo and Mosaico.
“We obviously feel bullish about the data in the ASCENT trial; otherwise, we would never go ahead with the efficacy trial,” says Larry Corey, MD, the principal investigator of HVTN.
In a previous nonhuman primate study, a vaccine similar to the Mosaico candidate protected 67% of the animals against infection. Researchers are hoping that in humans the vaccine will prove as effective and thus justify a global rollout.
Even a 50% HIV risk reduction from the vaccine would qualify it for prime time, says Fauci—even as he hopes for a higher rate. He explains that thanks to the power of PrEP and HIV treatment as prevention, a vaccine doesn’t need to be 95% effective. These three factors can complement each other and work synergistically to drive the epidemic into retreat.
“Every mathematical model shows you’d make a huge impact on the epidemic with a 50% effective vaccine,” Corey concurs.
Furthermore, says Fauci, “If Imbokodo gives good results, that would make me very optimistic that Mosaico would also.”

Anthony Fauci, head of NIAID, at CROI 2019 in SeattleBenjamin Ryan
Ideally, subsequent vaccine trials would build on such moderate success and produce next-generation vaccines that boast higher efficacy and thus can supplant the earlier versions.
Fauci notes that the Mosaico vaccine regimen is packed with all the elements that Imbokodo uses to prompt an immune response, with the exception that Mosaico has an extra element in the two booster shots—the last pair of injections. He’s referring to what are known as an additional mosaic of viral proteins—that’s where the trial’s name comes from—which investigators hope will make the Mosaico candidate even more robust and durable than its Imbokodo counterpart.
Hanneke Schuitemaker, PhD, vice president and head of viral vaccine discovery and translational medicine at Janssen Vaccines & Prevention, says she hopes this addition to the Mosaico regimen “will translate to broader protection against HIV” compared with the Imbokodo vaccine.
On the all-important subjects of access to and cost of an effective vaccine, Schuitemaker says, “We are, through our global health program, very much aware of the need to provide access to those in need, and that is really high on our agenda for our HIV vaccines.”
The ever-energetic Fauci, who is 15 months shy of 80 years old and who has been fighting HIV as an infectious disease doctor and public health leader since the epidemic’s official start in 1981, speculates about how he would react to a world that finally benefits from an effective vaccine for the virus.
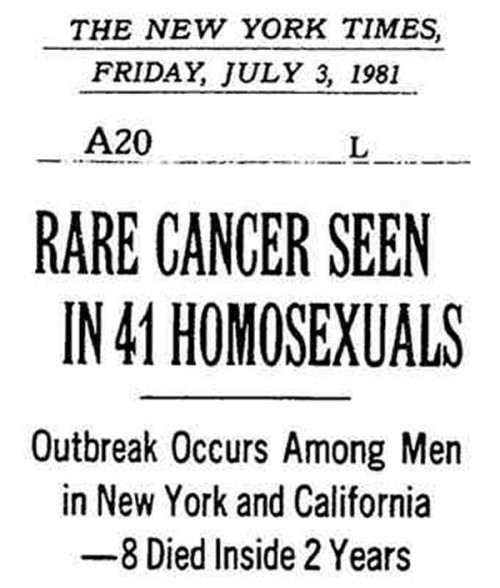
The first mention of the AIDS epidemic in The New York TimesTumblr
“It would be phenomenal,” Fauci says. “Then you could look back and say we started off with a brand new disease that didn’t have a name, didn’t have an etiology [an identified cause], didn’t have a treatment. To the point where we now have great treatments and then ultimately a vaccine—that would really be the icing on the cake.”
*****
Click here to read more about the technical makeup of the vaccine, including its use of a mosaic of viral proteins curated by a high-powered computer, and to learn more about the eligibility criteria for the trials.
Mosaico will likely launch U.S. recruitment in mid-October. If you are interested in participating, check out the trial’s ClinicalTrials.gov page and take note of the following:
- The “Recruitment Status” of the trial is on the top right-hand portion of the page.
- To find out whether there’s a study site near you, scroll down to “Contacts and Locations” and select the drop-down menu: “Show Study Locations.” Once the study is recruiting, you should see ways to contact each site.
- You can also call or email the “Study Contact” listed just above the drop-down menu.
A new website devoted to the trial will soon launch as well.







Comments
Comments