Even among people on antiretroviral treatment, cells in the viral reservoir continue to produce HIV genetic material and proteins that set off an ongoing immune response, potentially contributing to a host of health problems, according to three recent studies.
“No one actively questioned the presence of an active reservoir, but here [the researchers] find evidence that it might in fact matter,” long-time HIV cure researchers Steven Deeks, MD, of the University of California San Francisco, who was not involved in the research, told Science News.
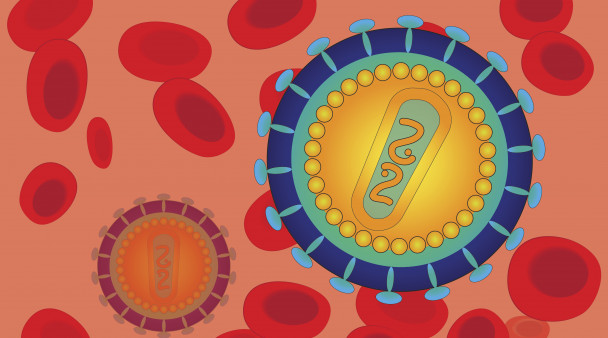
HIV inserts its DNA genetic blueprints into the chromosomes of human cells and establishes a long-lasting reservoir that antiretroviral drugs can’t reach. These so-called HIV proviruses can lie dormant indefinitely in resting T cells (mainly CD4 helper cells) during treatment, but they usually start churning out new virus when antiretrovirals are stopped, making a cure nearly impossible. Even among people with an undetectable viral load according to standard tests, persistent low-level virus can trigger chronic immune activation and inflammation, which can lead to conditions ranging from cardiovascular disease to cognitive impairment.
“It’s a deceptively dormant virus,” Daniel Kaufmann, MD, of the University of Lausanne and the University of Montreal Kaufmann, the senior investigator for one of the studies, said in a news release. “Even in people who are treated, HIV continues to have some activity, and it continues to interact with the immune system. We have to understand if these ongoing interactions have clinically relevant consequences.”
In the first study, published in the journal AIDS, Hiromi Imamichi, PhD, of the National Institute of Allergy and Infectious Diseases, and colleagues explored how defective nonreplicating HIV proviruses drive persistent immune activation and chronic inflammation.
This analysis included samples from 23 people with HIV. Fifteen were on antiretroviral therapy (ART) with viral suppression for an average of six years, while five samples were collected from people before treatment initiation. In addition, samples from three participants were collected over time since before they started ART.
The researchers measured HIV DNA, HIV RNA, HIV antibodies and key biomarkers of inflammation and coagulation (clotting) in peripheral blood. When the virus replicates, it first uses proviral DNA to make RNA templates (transcription), which are then used to produce viral proteins (translation).
They observed similar long-term persistence of multiple transcriptionally active HIV provirus clones and antibody responses against HIV proteins in all treated participants, regardless of viral load. What’s more, the participants sampled over time showed no change after starting treatment and achieving viral suppression. There was also little change in inflammatory biomarkers, including interleukin 6 and high-sensitivity C-reactive protein.
Although the proviruses were active, almost all appeared to be defective, or unable to produce functional virus. Nonetheless, people with greater transcription of defective proviruses had higher HIV antibody levels, and those with higher HIV DNA levels had more CD8 killer T cells, indicating ongoing immune activation. Higher levels of HIV RNA and proteins were also associated with elevated D-dimer, a biomarker of inflammation and coagulation.
“These findings suggest a novel interplay between transcription and translation of ‘defective’ HIV-1 proviruses and the persistent immune activation seen in the setting of treated chronic HIV-1 infection,” the study authors concluded.
In the second study, described in Cell Host and Microbe, Kaufmann and colleagues analyzed HIV persistence in 18 people on ART for more than three years, all of whom were white men.
Using various laboratory methods, the researchers detected active HIV transcription, or RNA production, in CD4 cells from 14 out of 18 people on ART. While these cells largely exhibited “abortive” transcription, indicating defective proviruses, seven participants (39%) had cells that expressed p24 and other HIV proteins. Even proviruses that were missing a substantial portion of their DNA could still produce viral proteins. What’s more, people with active reservoirs had stronger CD4 and CD8 T-cell immune responses.
“Our data suggest that the RNA and proteins produced by these viral reservoirs could be drivers of inflammation,” Kaufmann said. “This could be important because a subset of the people who are successfully treated with antiretroviral therapy for HIV still have negative consequences of living with the infection—for example, accelerated cardiac disease, frailty and premature osteoporosis.”
In a third study, described in the same journal, Lydie Trautmann, PhD, of the Vaccine and Gene Therapy Institute of Oregon Health and Science University and the U.S. Military HIV Research Program, and colleagues analyzed CD8 T cells from people who started ART during acute or chronic HIV infection. Before starting treatment, HIV-specific CD8 cells are dysfunctional and short-lived, the researchers noted as background.
The participants, almost all men, were drawn from two cohorts in Thailand. The analysis included 48 people who started treatment during acute, or very recent, infection and were on ART for at least two years, 17 people with chronic infection treated for at least two years and 17 people with chronic infection who had only been on ART for six months. The study population was relatively young, with a median age under 30 years, so it does not represent long-term survivors.
Here, too, a subset of participants’ CD4 cells continued to express HIV RNA despite antiretrovirals, though cells from those who started ART during acute infection produced fewer viral proteins. Both the size of the viral reservoir and the magnitude of CD8 T-cell responses declined after two years on treatment. Overall, people with sustained HIV-specific CD8 cell responses saw a greater reduction of integrated proviruses, but the magnitude of CD8 cells specific for HIV’s gag, pol, nef and vif proteins was associated with a larger active reservoir (measured as cell-associated viral RNA). High HIV DNA levels were strongly associated with maintenance of short-lived HIV-specific CD8 T cells, regardless of whether treatment was started during acute or chronic infection.
“Our data suggest that the active reservoir maintains HIV-specific CD8+ T cell magnitude but prevents their differentiation into functional cells,” the study authors concluded.
“Our study suggests that residual immune dysfunction driven by the active HIV reservoir on antiretroviral therapies could contribute to the lack of viral control after analytical treatment interruption by preventing the differentiation of functional stem-like self-renewing HIV-specific CD8+ T cells that can mount efficient rapid recall responses,“ they wrote. ”Therefore, HIV remission strategies will likely need to target transcriptionally active proviruses producing viral proteins during anti-retroviral therapies to harness HIV-specific CD8+ T cells to control rebounding of the virus after therapy cessation."
Click her for more news about HIV cure research.






Comments
Comments